Autologous blood therapy for osteoarthritis - ACP and PRP against joint pain
Can autologous blood therapy help me with osteoarthritis?
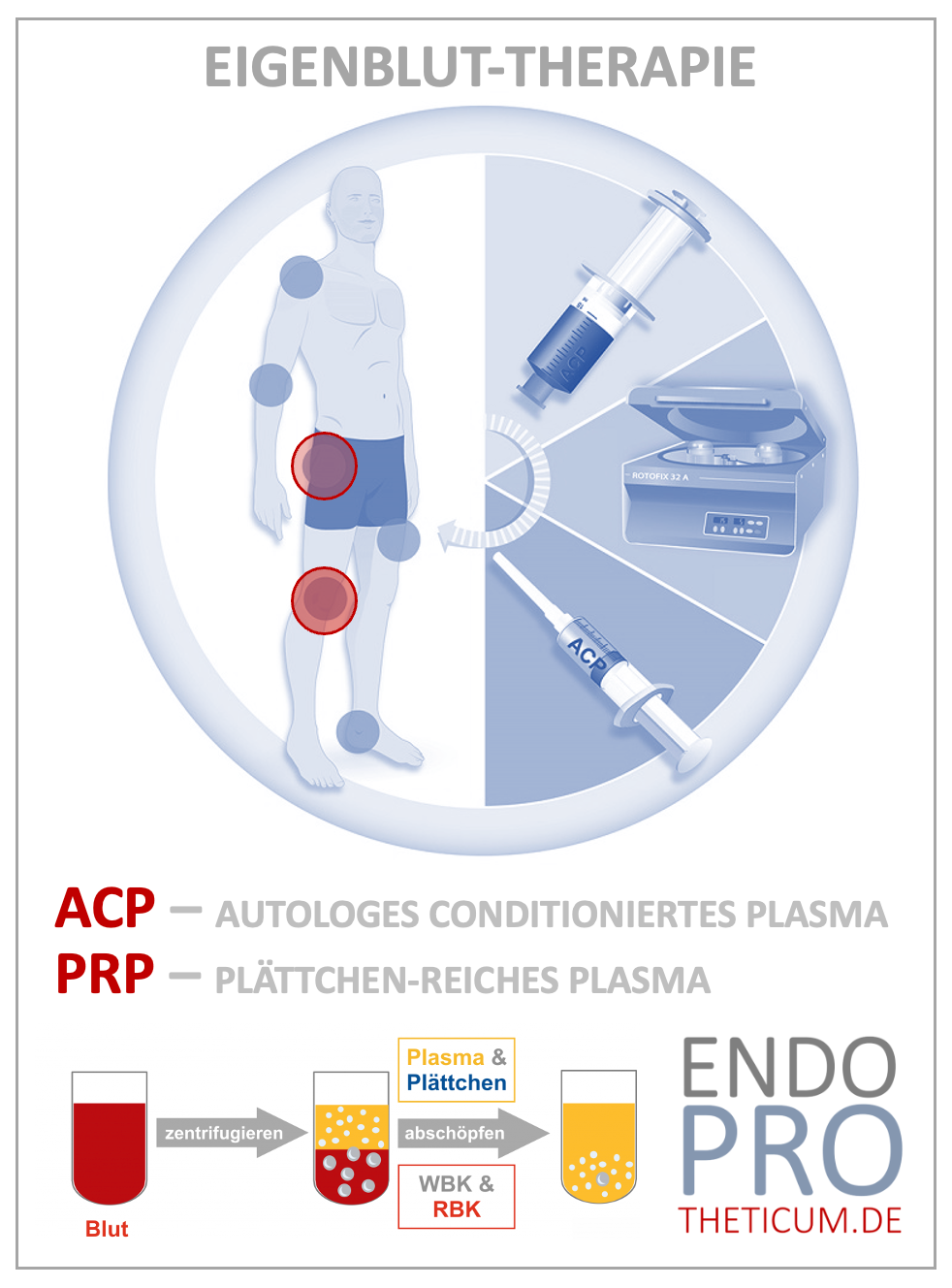
Autologous conditioned plasma (ACP) or platelet-rich plasma (PRP) therapy utilizes the body's own regenerative powers to alleviate osteoarthritis-related joint pain, particularly in the knee. This therapy is gaining popularity because it can reduce inflammation and relieve pain in osteoarthritis without the side effects of conventional medications. This article explores the scientific basis, advantages, and limitations of ACP and PRP treatment.
1. Basics of autologous blood therapy: ACP and PRP
In ACP/PRP therapy, a small amount of blood is drawn, processed, and the platelet-rich components are injected into the affected joint. The growth factors concentrated in the plasma promote the healing of cartilage and connective tissue. This method is particularly effective for osteoarthritis of the knee and other large joints, where the anti-inflammatory and regenerative effects are especially beneficial.
2. Applications and successes in the knee joint
ACP and PRP show particularly good efficacy in mild to moderate osteoarthritis of the knee joint. Studies and experience demonstrate that the therapy reduces pain, improves mobility, and alleviates inflammation-related swelling. ACP can serve as an alternative or complement to cortisone injections and painkillers to specifically treat inflammatory reactions.
3. Treatment procedure and typical dosages
A standard treatment plan typically consists of a series of three to five injections administered weekly. The procedure is simple and can be performed in a doctor's office. After blood is drawn, the plasma is processed and injected. Side effects are rare because only the patient's own material is used, thus minimizing the risk of allergic reactions.
4. Differences between ACP and PRP
Although both treatments are based on the same technology, they differ in their platelet content. ACP concentrates platelets less than PRP, making it a gentler alternative for milder joint pain and osteoarthritis. The choice between the two depends on individual needs and pain intensity.
How does ACP work?
The mechanism of action of ACP (Autologous Conditioned Plasma) therapy is based on the use of the body's own blood components, which initiate regenerative processes and support healing in arthritic or injured joints. ACP therapy works through the following mechanisms:
1. Increase in growth factor concentration
In ACP therapy, the patient's blood is centrifuged to separate the platelets and plasma from the red blood cells. These concentrated platelets contain a high number of growth factors (e.g., PDGF, VEGF, and TGF-β), which are injected into the affected joint. These growth factors promote cell proliferation, stimulating tissue repair and the formation of new cartilage cells.
2. Anti-inflammatory effect
Growth factors in ACP help modulate inflammatory responses. ACP can suppress the release of pro-inflammatory cytokines (such as TNF-alpha and interleukin-1) that contribute to pain and inflammation in osteoarthritis. Reducing these inflammatory mediators provides pain relief and slows the arthritic destruction of cartilage tissue.
3. Stimulation of collagen production
The platelets contained in ACP stimulate collagen production in cartilage tissue. Collagen is an important component of cartilage and contributes to the tissue's strength and flexibility. By promoting collagen synthesis, the cartilage tissue becomes more stable and resistant to stress.
4. Increased cartilage cell activity
The growth factors in ACP promote the activity of cartilage cells, which contributes to the maintenance and regeneration of damaged tissue. This is particularly important in degenerative joint diseases such as osteoarthritis, where cartilage cell activity decreases as the disease progresses.
5. Promoting tissue repair
The combination of the effects mentioned above promotes overall tissue repair. Increased cell proliferation, collagen production, and the anti-inflammatory effect ensure that damaged tissue regenerates more quickly. However, this is a supportive effect; ACP cannot completely compensate for cartilage loss, but it can slow the progression of osteoarthritis and alleviate symptoms.
These mechanisms make ACP a promising treatment method for osteoarthritis of the knee and other large joints, especially in mild to moderately advanced cases. Its effectiveness relies on stimulating the body's natural healing processes and is therefore particularly gentle and low-risk.
How does PRP work?
PRP (Platelet-Rich Plasma) therapy utilizes the properties of platelets and growth factors from the patient's own blood to support healing processes and alleviate joint pain, such as that caused by osteoarthritis. The mechanism of action of PRP is based on several important mechanisms:
1. Concentrated growth factors for regeneration
PRP is a highly concentrated mixture of blood platelets enriched with a high number of growth factors. These growth factors, such as PDGF (Platelet-Derived Growth Factor), EGF (Epidermal Growth Factor), and TGF-β (Transforming Growth Factor-Beta), promote cell proliferation and the formation of new tissue. They stimulate the growth of cartilage cells and contribute to the regeneration of damaged joint structures, particularly in degenerative conditions such as osteoarthritis
2. Stimulation of collagen production
PRP promotes the production of collagen, an important component of cartilage tissue that supports the tissue's stability and flexibility. The increased collagen synthesis helps make the cartilage more resistant to stress, which is essential for joint stability and function.
3. Modulation of the inflammatory response
PRP helps control inflammatory processes. The platelets release anti-inflammatory molecules that suppress the production of pro-inflammatory cytokines (such as IL-1 and TNF-alpha). This anti-inflammatory effect can reduce pain in osteoarthritis and slow the progression of the disease, which is particularly helpful for patients with chronic inflammation.
4. Promotion of cell migration and angiogenesis
Growth factors in PRP promote cell migration and angiogenesis (formation of new blood vessels). This improves the supply of nutrients and oxygen to the cartilage and surrounding tissues. Especially in joints like the knee, which has limited blood flow, improved blood supply can stimulate healing processes and contribute to faster regeneration.
5. Stimulating cartilage cell proliferation
PRP also contains bioactivators that stimulate cartilage cells to divide and produce healthy cartilage tissue. Since osteoarthritis is often accompanied by a loss of functional cartilage, this effect of PRP treatment can slow the progression of osteoarthritis and contribute to pain reduction.
6. Structural support and protection of the joint
In cases of osteoarthritis of the knee, PRP helps to stabilize the affected joint and make it less susceptible to microtrauma caused by everyday stress. It thus protects against further damage and creates an environment that supports the long-term functionality of the joint.
PRP therapy is a minimally invasive treatment method that is particularly well-suited for patients with mild to moderate osteoarthritis symptoms. It is highly safe, as it uses only the patient's own substances, and therefore carries a low risk of allergic reactions and infections.
Limits and risks of autologous blood therapy
ACP/PRP therapy is not a miracle cure and is not suitable for every patient. Success is limited in cases of severe cartilage damage or advanced osteoarthritis, as the treatment cannot fully regenerate the tissue. Patients should have realistic expectations and consider autologous blood therapy as part of a comprehensive treatment plan.
MAKE AN APPOINTMENT?
You are welcome to make an appointment either by phone or online .