Artificial hip joint: The most successful operation of the century
The operation of the century: artificial hip joint
The implantation of an artificial hip joint, also known as a total hip arthroplasty (THA), is often described as the most successful operation of the century. This medical innovation has helped countless people around the world regain mobility and significantly improve their quality of life. This comprehensive blog post details the history, techniques, materials, benefits and potential complications of hip replacements and explains why this surgery is considered revolutionary.
History of the artificial hip joint
The development of the artificial hip joint dates back to the 1960s, when Sir John Charnley developed the modern hip prosthesis. This early form of artificial hip joint consisted of a metal ball and a polyethylene socket. This invention was groundbreaking and laid the foundation for today's hip arthroplasty, which has been constantly further developed.
The history of the artificial hip joint is a fascinating journey through the development of modern medicine and surgery.
Early attempts and developments (19th century)
- The first attempts to replace damaged joints date back to the 19th century. Surgeons experimented with ivory and various metals to replace parts of the hip joint, but with limited success due to a lack of biocompatibility and high infection rates.
Sir John Charnley and the modern THA (1960s)
- The British orthopedist Sir John Charnley achieved a decisive breakthrough in the 1960s. Charnley developed the first modern artificial hip joint, consisting of a metal ball and a polyethylene socket. This combination offered better durability and lower friction, resulting in a significant improvement in functionality.
- Charnley's innovation also involved the use of bone cement (polymethyl methacrylate) to anchor the prosthesis into the femur. This method significantly increased the stability and longevity of the implants.
Further development of materials (1970s to 1980s)
- In the following decades, the materials and designs were continuously developed. Titanium and ceramic were introduced to improve biocompatibility and increase abrasion resistance. These advances resulted in longer implant lifespan and reduced the risk of complications such as prosthesis loosening and abrasion.
- The introduction of cementless implantation in the 1980s, in which the implant has a porous coating that promotes bone tissue ingrowth, represented a significant advancement. This increased stability and reduced the need for bone cement.
Minimally invasive surgery and modern techniques (1990s to present)
- The 1990s brought the introduction of minimally invasive surgical techniques that accelerated the healing process and reduced postoperative pain. These techniques, such as the anterior approach, allow for smaller incisions and protect the surrounding tissue, resulting in faster rehabilitation.
- The use of computer and robotic navigation systems has further increased the precision of implantations. These technologies allow for more precise implant placement, improving functionality and reducing the risk of misalignment.
Endoprosthesis register and quality assurance
- The introduction of endoprosthesis registries, such as the EPRD in Germany, has made it possible to systematically record and evaluate the long-term results of hip prostheses. This data helps identify best practices and continuously improve implantation techniques and materials.
Techniques and methods
When implanting an artificial hip joint, various surgical approaches are available, including the minimally invasive anterior approach, the lateral approach and the posterior approach. The minimally invasive anterior approach is particularly advantageous because it does not cut the muscles but pushes them to the side. This technique reduces postoperative pain and accelerates rehabilitation, making patients mobile again more quickly.
Materials and design
Modern artificial hip joints are made of high-quality materials such as titanium, ceramic and polyethylene. These materials are biocompatible and are characterized by their longevity and low tendency to abrasion. The design of the artificial hip joint is carefully adapted to the individual anatomy of the patient to ensure optimal functionality and durability.
Properties of an artificial hip joint
- Materials: Modern artificial hip joints are made of high-quality materials such as titanium, ceramic and polyethylene. These materials are biocompatible and are characterized by their longevity and low tendency to abrasion.
- Design: The design of an artificial hip joint is complex and is adapted to the individual anatomy of the patient. A typical hip joint consists of a shaft that is implanted into the femur and a ball that fits into a socket in the pelvic bone. This allows for smooth movement similar to that of a natural hip joint.
- Sliding pairings: Sliding pairings refer to the materials that slide on each other in the joint surface. Common combinations include metal on polyethylene, ceramic on ceramic and ceramic on polyethylene. Modern ceramics and highly cross-linked polyethylene offer better abrasion properties and reduce the risk of particle abrasion, which can lead to complications.
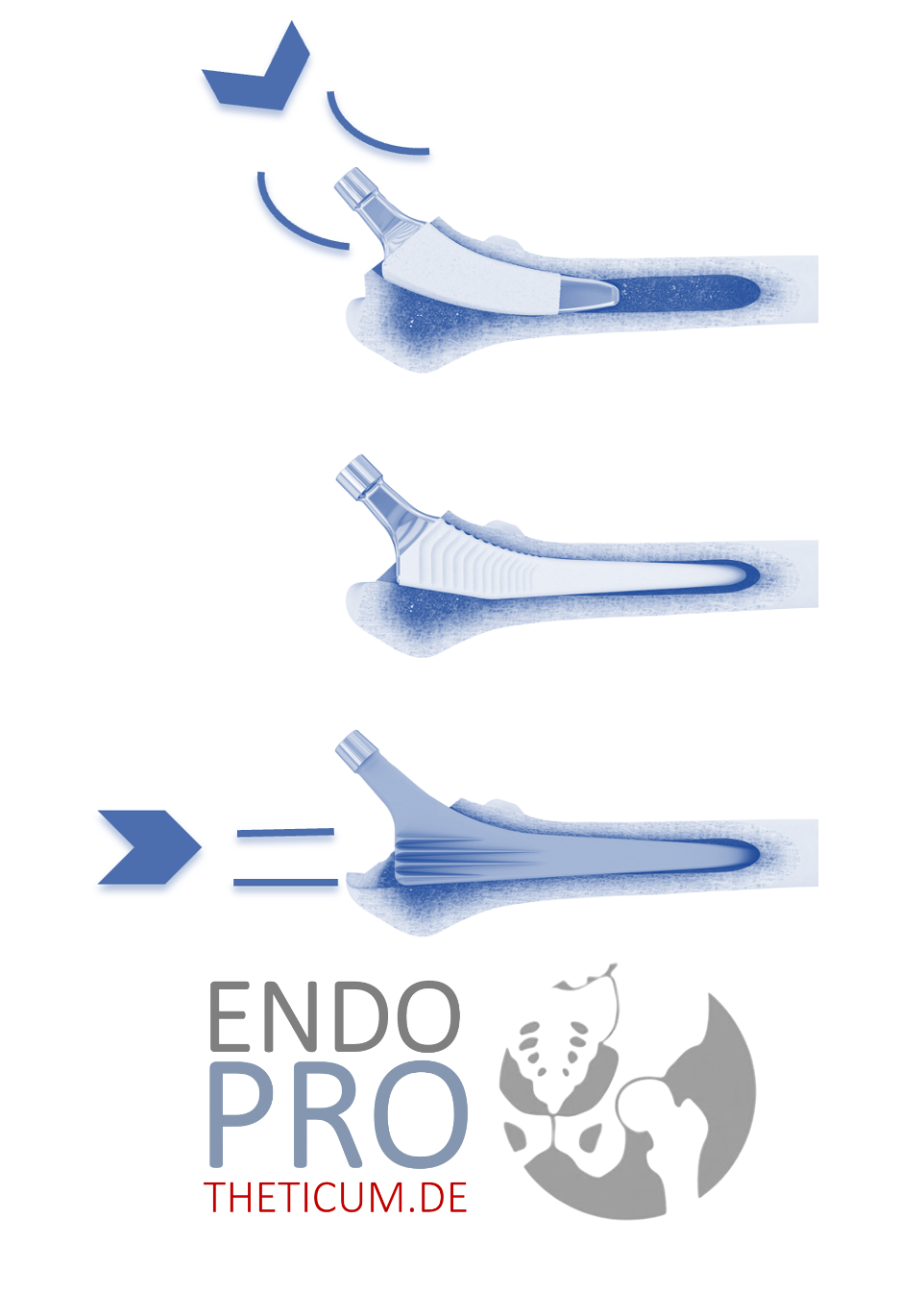
- Fixation: Artificial hip joints can be fixed either without cement or with cement. Cementless implants are often coated to promote bone ingrowth and create a stable connection. Cemented implants use a special bone cement for fixation.
- Minimally invasive techniques: Minimally invasive approaches, such as the anterior approach, have revolutionized hip arthroplasty. These techniques minimize tissue damage, reduce postoperative pain, and significantly shorten recovery time. Smaller skin incisions and gentler procedures further reduce the risk of complications.
Advantages of the artificial hip joint
An artificial hip joint offers numerous advantages:
- Pain Relief: Patients typically experience a significant reduction in their pain.
- Improved mobility: The artificial hip joint allows for a significant improvement in freedom of movement and functionality.
- Long lifespan: With modern materials, an artificial hip joint can last 15 to 20 years or longer, depending on the patient's individual circumstances and activity level.
Complications and risks
As with any operation, there are risks and possible complications when implanting an artificial hip joint. These include infections, loosening of the prosthesis, dislocations and wear of material. However, thanks to modern techniques and materials, the likelihood of such complications is relatively low.
The role of rehabilitation measures
Rehabilitation is crucial to the long-term success of an artificial hip joint. Physiotherapy begins on the first day after the operation to promote mobility and strengthen the muscles. Intensive aftercare and regular checks help to maximize the functionality and lifespan of the artificial hip joint.
Minimally invasive techniques and their advantages
Minimally invasive techniques, such as keyhole surgery, have revolutionized the implantation of an artificial hip joint. These methods minimize tissue damage, reduce postoperative pain, and significantly shorten recovery time. Smaller skin incisions and gentler procedures further reduce the risk of complications.
Future prospects
The future of hip arthroplasty is promising. Research and development focuses on improving materials, optimizing surgical techniques and customizing prostheses. As technology and medical knowledge advances, outcomes for hip replacement patients continue to improve and prosthetic lifespan is extended.
Conclusion
The implantation of an artificial hip joint has established itself as the most successful operation of the century. Thanks to innovative techniques, modern materials and careful aftercare, millions of people worldwide can lead a pain-free and mobile life. Continuous research and development in this area promises an even better future for patients with hip problems.
MAKE AN APPOINTMENT?
You are welcome to make an appointment either by phone or online .