Artificial hip joint: When is the right time?
What "red flags" indicate the need for an artificial hip joint?

Deciding on a hip replacement is one of the most important steps in the treatment of hip joint disorders. For many affected individuals, this raises fundamental questions: When is the right time for surgery? What are the "red flags" that necessitate an operation? And why is it often not advisable to wait until the "last minute" for surgery these days?
This blog explains how to recognize that an artificial hip joint is necessary, what factors influence the decision, and why modern endoprostheses have changed the perspective on this important operation.
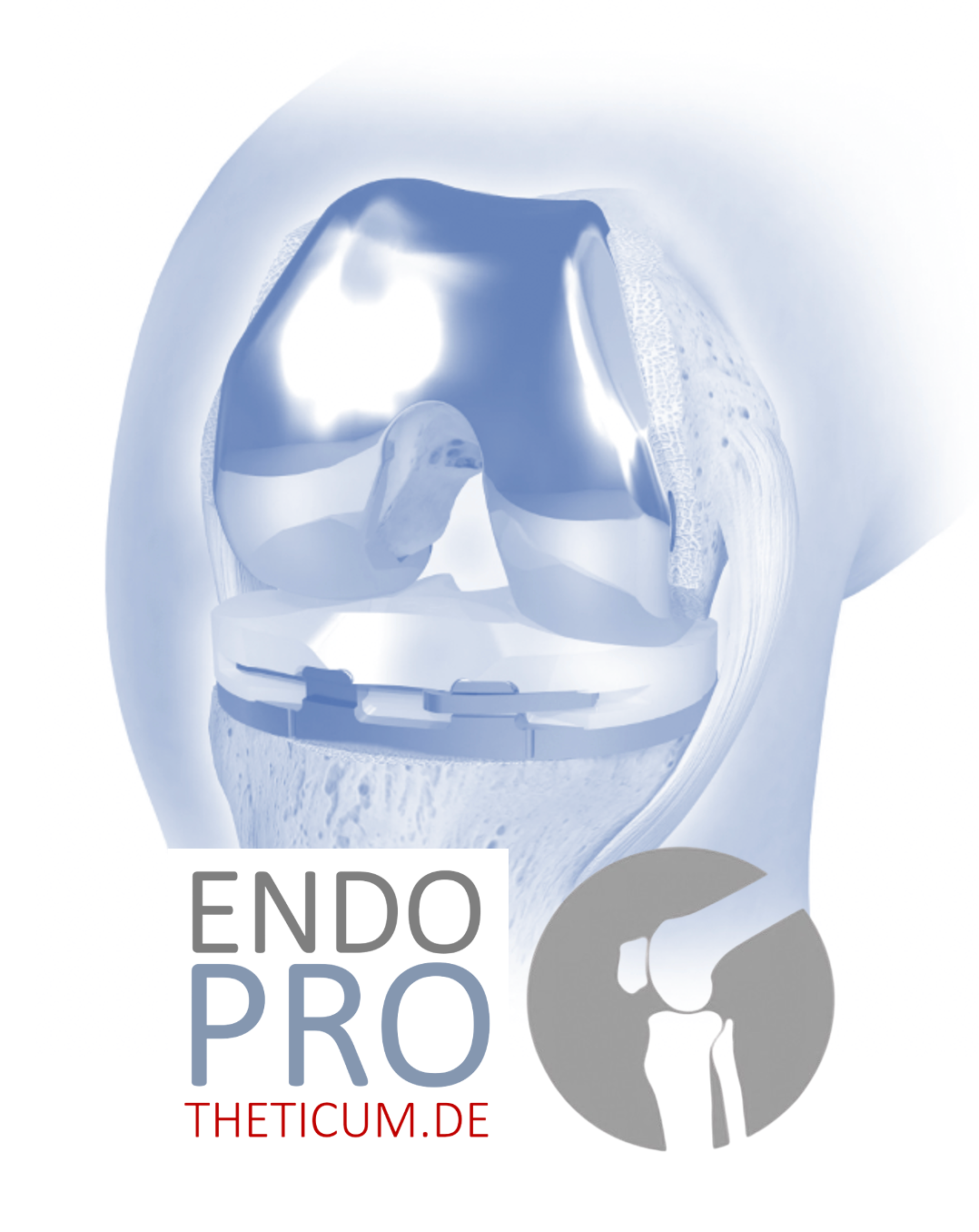
What is an artificial hip joint?
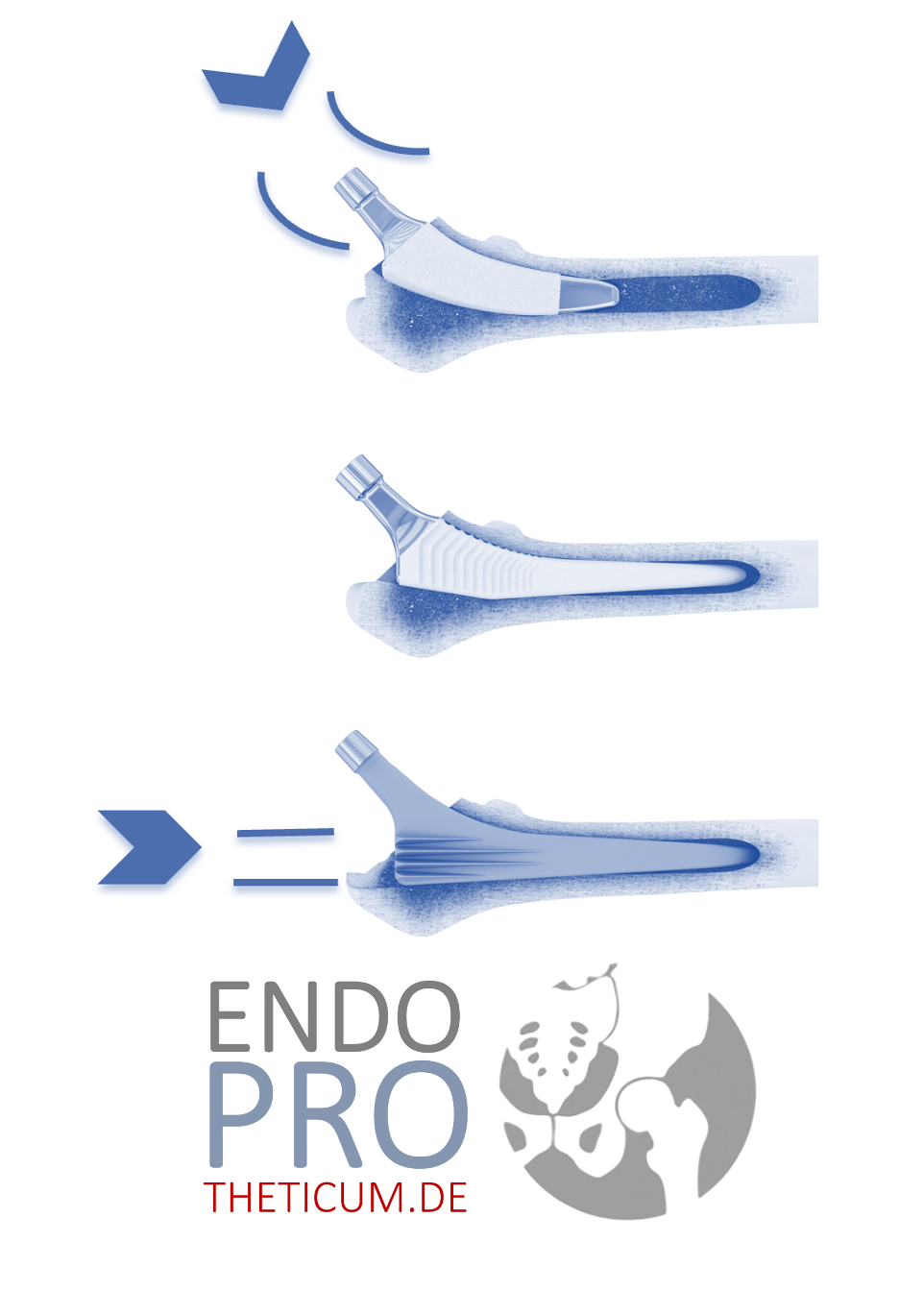
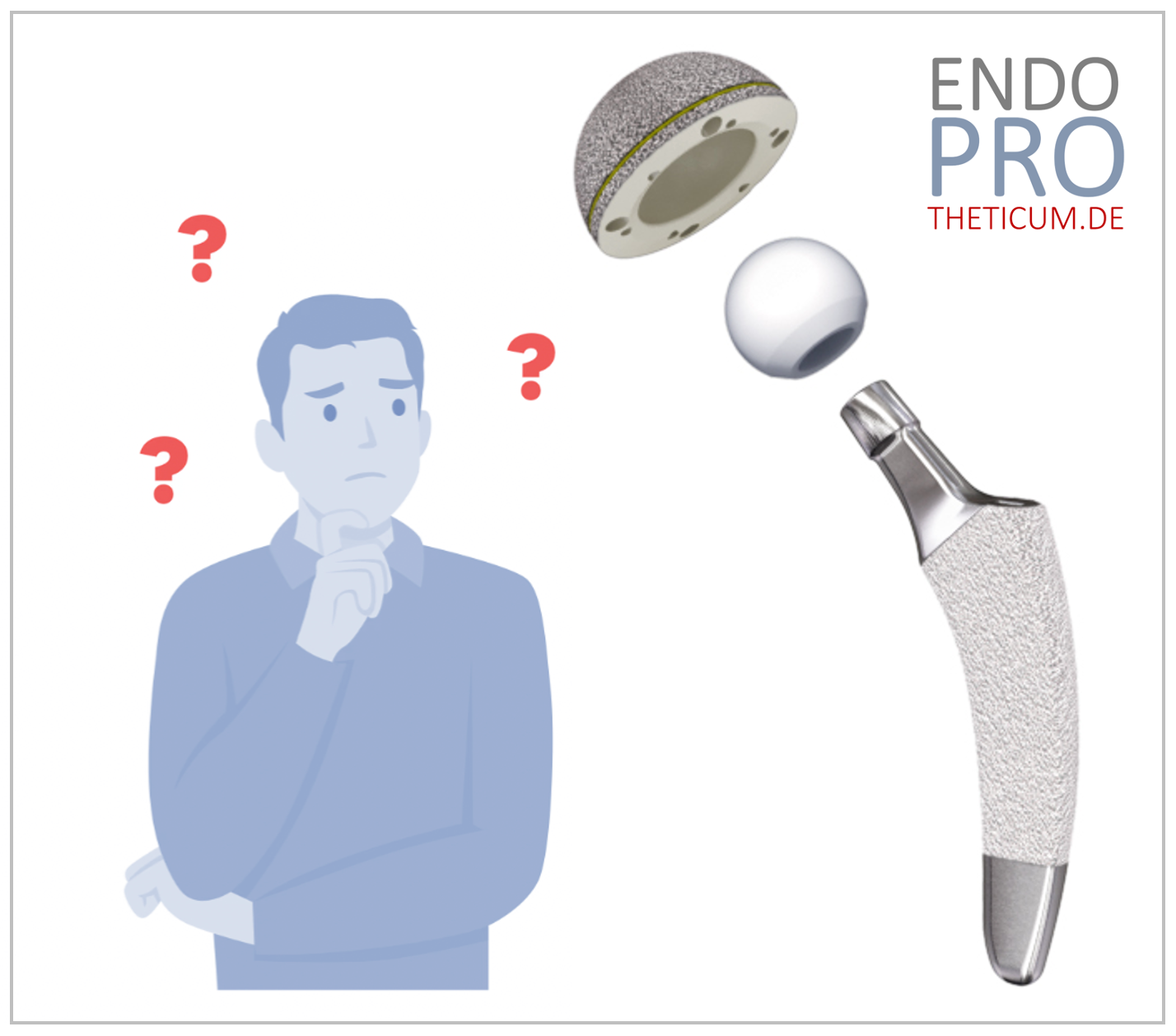
An artificial hip joint, also known as a total hip replacement (THR) , is an implant that replaces the natural hip joint. It consists of a ball-shaped head (which replaces the femoral head) and a socket (which replaces the acetabulum of the pelvis). Modern prostheses are made of durable materials such as:
- Ceramic (highly abrasion-resistant and biocompatible)
- Titanium (robust and lightweight)
- Polyethylene with added vitamin E (low wear and stable)
The goal of an artificial hip joint is to restore mobility, freedom from pain, and quality of life.
Symptoms and signs: When is an artificial hip joint necessary?
So-called "red flags" help identify whether hip surgery is necessary. These signs can indicate critical wear and tear of the hip joint and should be taken seriously. Here are the most important warning signs:
1. Chronic pain
Persistent pain in the hip region, even during rest or at night, is a major sign of a serious joint condition. Particularly typical symptoms include:
- Groin pain: Pain in the groin area or thigh that increases with walking movements.
- Radiating pain: Discomfort that radiates into the knee or lower back.
2. Mobility restrictions
Loss of mobility is a clear indication of a progressive disease:
- Flexion restriction: Problems lifting the leg or bending it at an angle greater than 90°.
- Rotational discomfort: Difficulty getting in and out of the car or putting on shoes.
3. Muscle loss
Pain-induced protective postures often lead to a significant loss of muscle mass around the joint. This muscle weakness can further impair stability and lead to postural problems.
4. X-rays and diagnosis
An X-ray can reveal the extent of joint damage. Typical signs include:
- Loss of joint space: A significant reduction or complete loss of the joint space indicates advanced cartilage wear.
- Osteophyte formation: Bone growths that result from chronic inflammation.
- Bone damage: Cystic changes in the bone.
5. Functional limitations in everyday life
Anyone who can no longer manage everyday activities such as walking, climbing stairs or shopping without help due to pain or limited mobility should consider a surgical solution.
Modern endoprostheses: Why waiting is often no longer advisable
Previously, the prevailing wisdom was to postpone joint replacement for as long as possible. This was due to the limited lifespan of implants, which was estimated at 10 to 15 years. However, with today's advances in materials science, this approach has fundamentally changed.
Increased durability of modern materials
Thanks to the development of abrasion-resistant materials, hip implants can now last up to 25 years or longer. These include:
- Vitamin E-stabilized polyethylene: Protects against oxidation and abrasion.
- Ceramic-on-ceramic bearing pairs: Reduce particle formation and offer excellent biocompatibility.
- Titanium anchorage: Promotes ingrowth into the bone.
Advantages of early intervention
Timely intervention offers crucial advantages:
- Preserving muscle mass: Early replacement prevents the surrounding muscles from deteriorating, which accelerates rehabilitation.
- Fewer long-term consequences: Chronic pain and compensatory postures lead to misalignments, which can be avoided through early treatment.
- Better surgical outcomes: The probability of an optimal result is higher if the joint is not yet completely destroyed.
Individual risk-benefit assessment for artificial hip joints
Although hip replacement technology is now highly advanced, the decision remains individual and should be made in close consultation with an experienced specialist. The following aspects are taken into consideration:
1. General health
Patients with good general health parameters, such as a stable cardiovascular system, have a lower risk of complications.
2. Activity level and lifestyle
Younger, active patients often benefit particularly from early interventions, as they regain a high level of mobility and quality of life after the surgery.
3. Progression of osteoarthritis
Depending on the severity of the osteoarthritis and the symptoms, the right time for surgery can vary. Moderate stages are better suited for planned procedures.
4. Mental preparation
The patient's willingness to actively participate in rehabilitation is essential for the success of the operation.
Conclusion: When is the right time for an artificial hip joint?
A hip replacement restores quality of life and relieves chronic pain. Thanks to modern materials and surgical techniques, it's no longer necessary to postpone surgery until the last minute. Pay attention to your body's signals and consult an experienced specialist to determine the optimal time for you.
Don't hesitate to seek medical help if you experience persistent symptoms. A timely decision to have an intervention can save you pain and restore you to an active life.
Conclusion: Pay attention to the "red flags"
Waiting until the very last minute to decide on a hip replacement is no longer advisable. Those who react to warning signs early benefit from improved surgical techniques, longer-lasting prostheses, and a higher quality of life.
Listen to your body's signals – and if you experience persistent discomfort, consult a hip surgery specialist to determine the right time for your individual therapy.
MAKE AN APPOINTMENT?
You are welcome to make an appointment either by phone or online .