Periprosthetic fractures in short stem prostheses - What is the risk?
Do short-stem prostheses offer advantages with regard to periprosthetic fractures?
An artificial hip joint improves the quality of life for millions of people worldwide. However, despite all the advances in endoprosthetics, complications can occur, including so-called periprosthetic fractures. These fractures in the immediate vicinity of the prosthesis can arise for various reasons and pose a significant challenge for both physicians and patients. Particularly with short-stem prostheses, specific biomechanical factors that influence the fracture risk must be considered. In this article, we examine in detail the causes, diagnosis, treatment options, and prevention of periprosthetic fractures in short-stem prostheses.
What are periprosthetic fractures?
Periprosthetic fractures are bone fractures that occur in the area of an already implanted artificial joint. These fractures typically occur around the prosthesis stem fixation and can occur both intraoperatively and postoperatively.
Classification of periprosthetic fractures
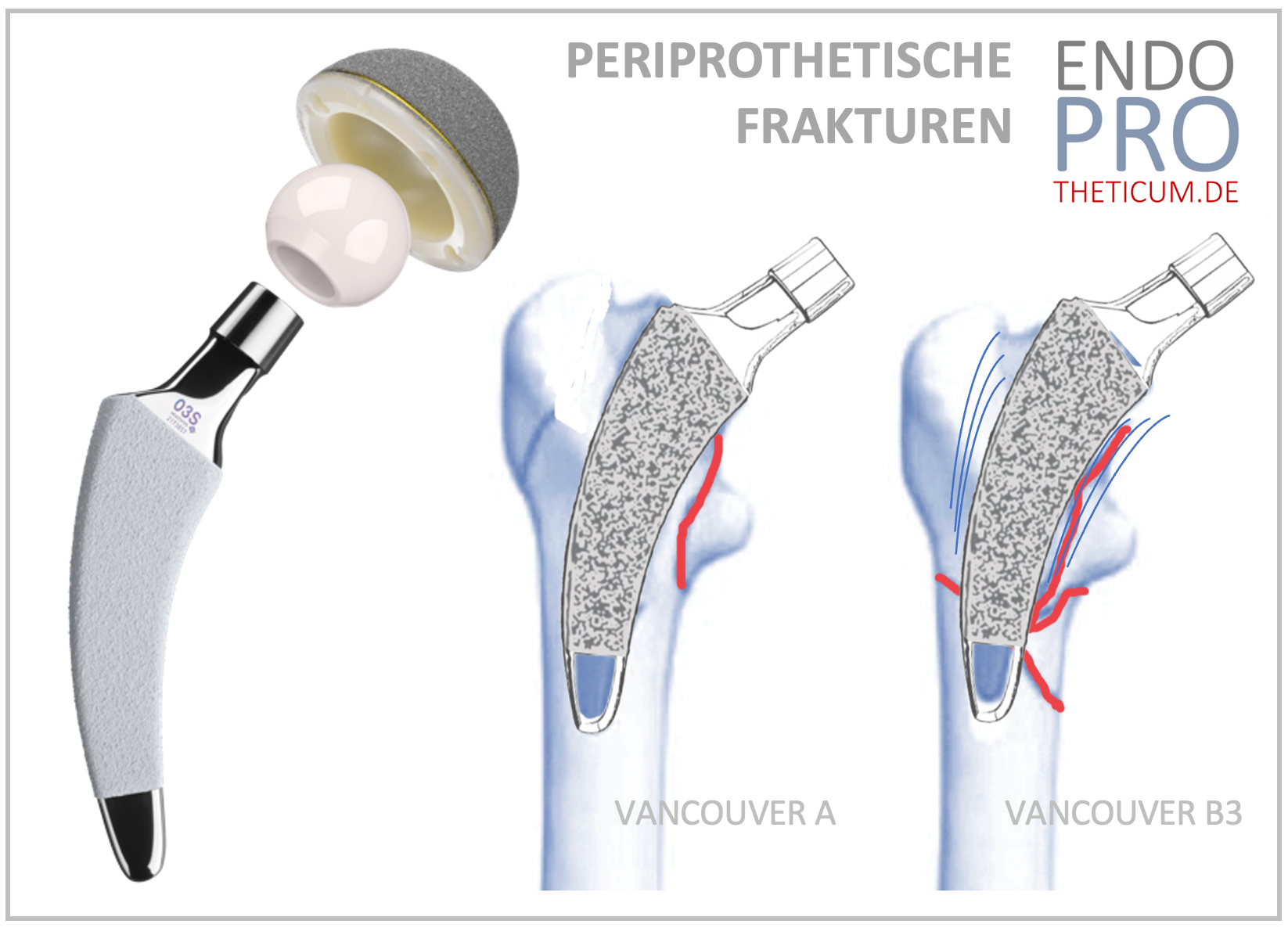
Periprosthetic fractures are classified according to various systems. The commonly used Vancouver classification system divides fractures into:
- Type A : Fractures of the greater or lesser trochanter (usually treatable conservatively)
- Type B1 : Fractures in the area of the prosthesis stem with a stable prosthesis
- Type B2 : Fractures with loosening of the prosthesis
- Type B3 : Fractures with poor bone quality
- Type C : Fractures below the prosthesis stem
Distinguishing between these fracture types is crucial for choosing the appropriate treatment method.
Why do fractures occur with short-stem prostheses?
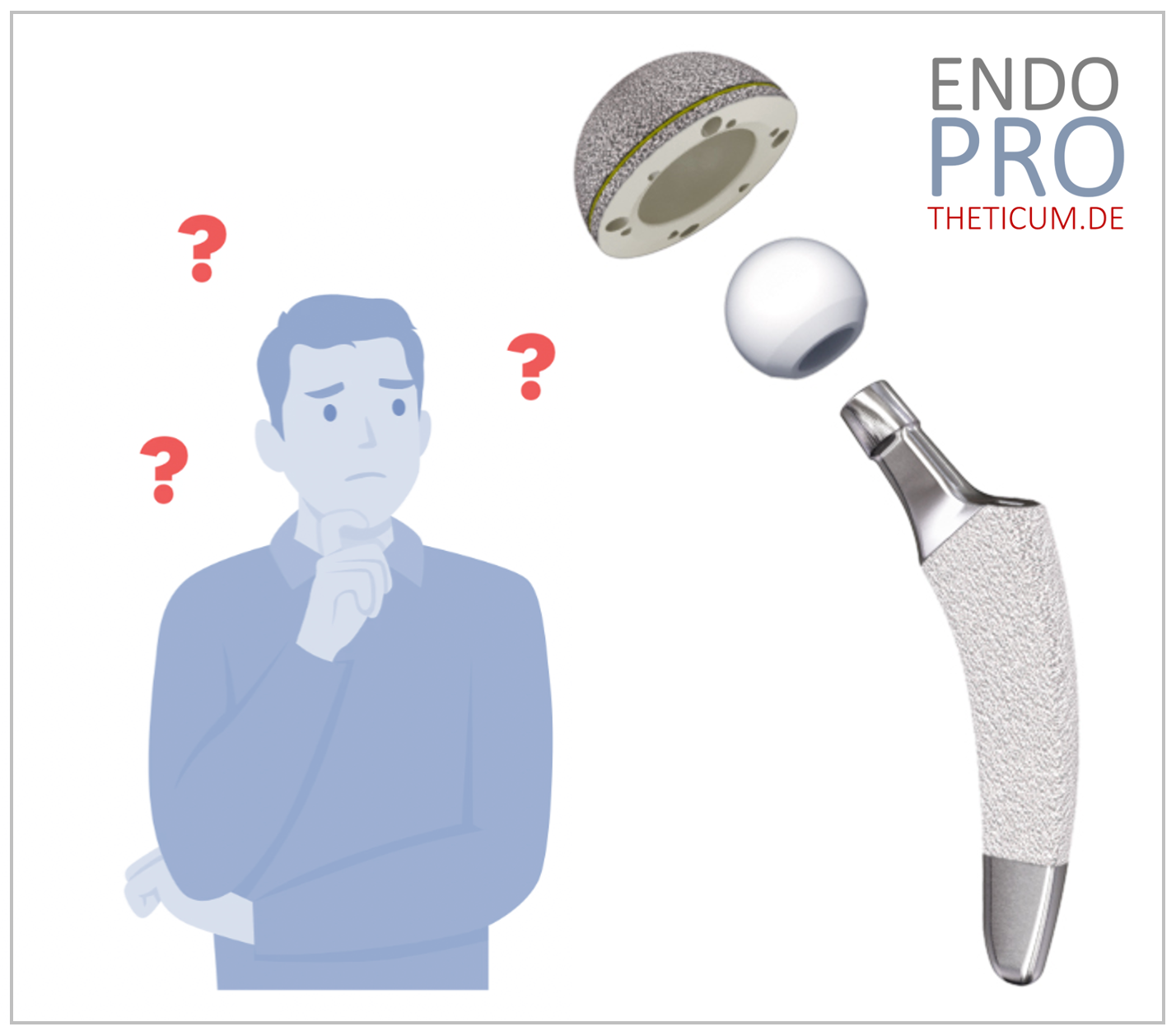
Short-stem prostheses are designed to allow for implantation that conserves bone as much as possible. Fixation occurs primarily in the proximal femur, resulting in a different distribution of load and force compared to conventional long-stem prostheses.
Factors that increase the risk of fracture:
- Incorrect loading after surgery : Incorrect loading in the first weeks after implantation can increase the risk of microfractures.
- Insufficient primary anchorage : A poor fit or suboptimal positioning of the implant can impair bone stability.
- Patient's age and bone density : Patients with osteoporosis have a higher risk of periprosthetic fractures.
- Falls and trauma : Direct impacts or falls can cause a fracture in the area of the prosthesis.
Risk factors for periprosthetic fractures in short-stem prostheses
Patient-related factors:
- Osteoporosis or other diseases with reduced bone density
- Old age
- Lack of muscle mass and poor balance
- Inadequate postoperative rehabilitation
Implant-related factors:
- Insufficient bony integration of the prosthesis
- Choosing a prosthesis that is too small or too large
- Use of a design that is not optimally suited to the patient
Surgical factors:
- Careless intraoperative manipulation of the bone
- Inadequate fixation of the prosthesis
- Use of unsuitable access routes (minimal versus conventional incisions)
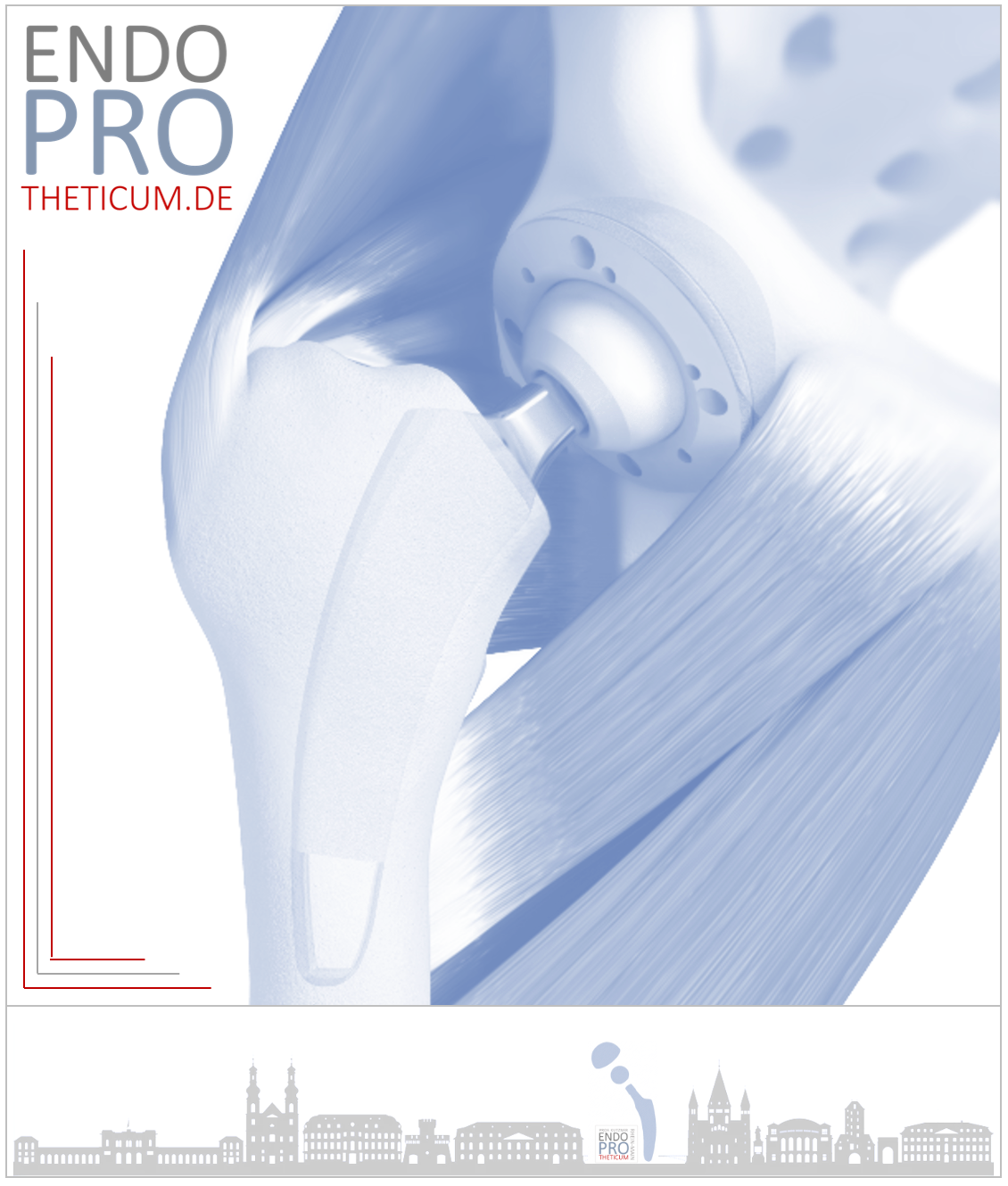
Differences in periprosthetic fractures between short stems and straight stems
1. Different anchorage in the bone
- Short-stem prostheses are anchored in the metaphysis, i.e., in the upper part of the femur. This leaves the diaphysis (the long tubular part of the femur) largely intact.
- Straight stem prostheses, on the other hand, extend deeper into the diaphysis and are firmly anchored there.
This different anchoring influences the type of fractures:
- With short stem prostheses, fractures tend to occur in the proximal (upper) thigh area , especially if the metaphyseal anchoring is not optimal.
- With straight-stem prostheses, fractures often occur in the diaphysis , that is, further down on the femur. These fractures are more difficult to treat, as they often require re-anchoring the implant at a deeper depth.
2. Stability and bone reserves
- One advantage of short-stem prostheses is that the shorter anchorage in the bone preserves more bone substance. This can be helpful in the case of a fracture, as more bone material is available for surgical stabilization.
- With straight stem prostheses, a periprosthetic fracture can be more critical because the bone structure has been altered more due to the long anchoring time and there are often fewer bone reserves available.
3. Risks associated with falls and accidents
- Straight stem prostheses increase the risk of distal fractures (lower femur fractures) because the rigid, long anchoring transfers leverage forces to the lower part of the femur.
- Short stem prostheses generally have a lower risk of such distal fractures because they are shorter and the force is limited to a smaller bone region.
4. Treatment options for fractures
- In cases of fractures around a short stem prosthesis , it is often possible to treat them with plate osteosynthesis or other stabilizing measures without having to replace the prosthesis.
- In cases of fractures around a straight stem prosthesis, a change to a longer-reaching, axis-guided or modular revision prosthesis is often necessary.
5. Are short-stem prostheses advantageous?
- Short-stem prostheses show a lower risk of serious diaphyseal fractures because the bone structure is largely preserved.
- When fractures do occur, they usually happen near the proximal bone , which offers better treatment options.
- In contrast, straight stem prostheses have a higher risk of fractures in the middle and lower thigh area , which are more difficult to treat.
Overall, short stem prostheses offer certain advantages with regard to periprosthetic fractures, especially concerning bone preservation and treatment options in the event of a fracture.
Diagnosis of a periprosthetic fracture
A quick and accurate diagnosis is essential to initiate appropriate treatment. Typical symptoms include sudden pain, swelling, and restricted movement of the affected leg.
Diagnostic procedures:
- X-rays to locate the fracture
- Computed tomography (CT) for better visualization of fractures and implant position
- Magnetic resonance imaging (MRI) in cases of suspected soft tissue injuries
Treatment options for periprosthetic fractures
The therapy depends on the fracture type, the stability of the prosthesis, and the patient's bone quality.
Conservative therapy
- Only applicable to stable fractures without prosthesis loosening
- Immobilization through partial weight-bearing and physiotherapy
Surgical therapy
- Osteosynthesis : Screw fixation or plate osteosynthesis for stable prostheses
- Revision prosthesis : If the prosthesis is loose or there is massive bone damage.
- Bone transplantation or augmentation procedures : In cases of severe osteoporosis or bone loss
Prevention of fractures in short-stem prostheses
Since periprosthetic fractures represent serious complications, preventive measures are essential.
Choosing the right implant
- Individual adaptation to the patient's bone anatomy
- Use of modern implants with optimized anchoring
Optimizing bone density
- Osteoporosis medication and vitamin D supplementation
- Strength training to strengthen muscles
Patient behavior after surgery
- Preventing falls through balance training
- Adherence to the recommended postoperative activity limits
Conclusion and recommendation
Periprosthetic fractures represent a serious complication in endoprosthetics. Especially with short-stem prostheses, individual patient adaptation is crucial to minimize the risk. Modern implants and improved surgical techniques have reduced the incidence of such fractures; however, precise diagnosis and treatment remain essential.
Patients who need a hip replacement or already have an implant should consult specialized centers to achieve the best possible results. The combination of precise surgical technique, high-quality implant selection, and tailored rehabilitation minimizes the risk of complications and improves long-term outcomes for the patient.
MAKE AN APPOINTMENT?
You are welcome to make an appointment either by phone or online .