Osteoarthritis of the hip (coxarthrosis) - everything you need to know
A common disease: Osteoarthritis of the hip joint (coxarthrosis)

What is osteoarthritis of the hip (coxarthrosis)?
Osteoarthritis of the hip, also known as coxarthrosis, is one of the most common forms of osteoarthritis and affects the hip joint. It is a degenerative disease in which the articular cartilage is progressively broken down. Articular cartilage ensures smooth movement and absorbs stress on the hip joint. When this cartilage is worn away, pain, stiffness, and loss of function result.
Anatomy of the hip joint
The hip joint is a ball-and-socket joint consisting of the spherical head of the femur and the socket in the pelvis. It is covered by a protective layer of cartilage that facilitates joint movement.
Why is the hip joint prone to osteoarthritis?
Since the hip joint bears the entire body weight and is subject to high mechanical loads, it is particularly susceptible to wear and tear such as osteoarthritis.
Causes of hip osteoarthritis
The causes of coxarthrosis can be divided into primary and secondary factors.
1. Primary osteoarthritis
- Age-related wear and tear: As we age, cartilage loses elasticity.
- Genetic predisposition: A family history of the condition can increase the likelihood.
2. Secondary osteoarthritis
- Injuries: Previous fractures or dislocations.
- Inflammatory diseases: Rheumatoid arthritis.
- Anatomical malformations: Congenital hip dysplasia.
- Incorrect loading: leg length discrepancies or excess weight.
Risk factors
- Obesity: Excess weight puts excessive strain on the joint.
- Occupational stress: Heavy lifting.
- Sports overuse injuries: Especially sports with high jumping loads.
Symptoms of hip osteoarthritis
1. Pain
- Pain in the groin, buttocks, or thigh.
- Initially, pain was dependent on exertion; later, pain also occurred at rest.
2. Stiffness and restricted movement
- Stiffness after getting up or after prolonged inactivity.
- Difficulty putting on shoes or climbing stairs.
3. Other symptoms
- Joint noises when moving.
- Muscle loss.
Diagnosis of osteoarthritis of the hip joint
1. Medical history: A detailed discussion with the doctor about your symptoms.
2. Clinical examination
- Joint mobility test.
- Pressure pain tests.
3. Imaging
- X-ray: Visualization of cartilage thickness.
- MRI: Used in unclear cases for the precise examination of cartilage and soft tissues.
- Ultrasound: Diagnosis of joint effusions.
Treatment of hip osteoarthritis
1. Conservative therapy
- Medications: NSAIDs, cortisone injections.
- Physiotherapy: Building up the surrounding muscles.
- Hyaluronic acid: Promotes lubrication in the joint.
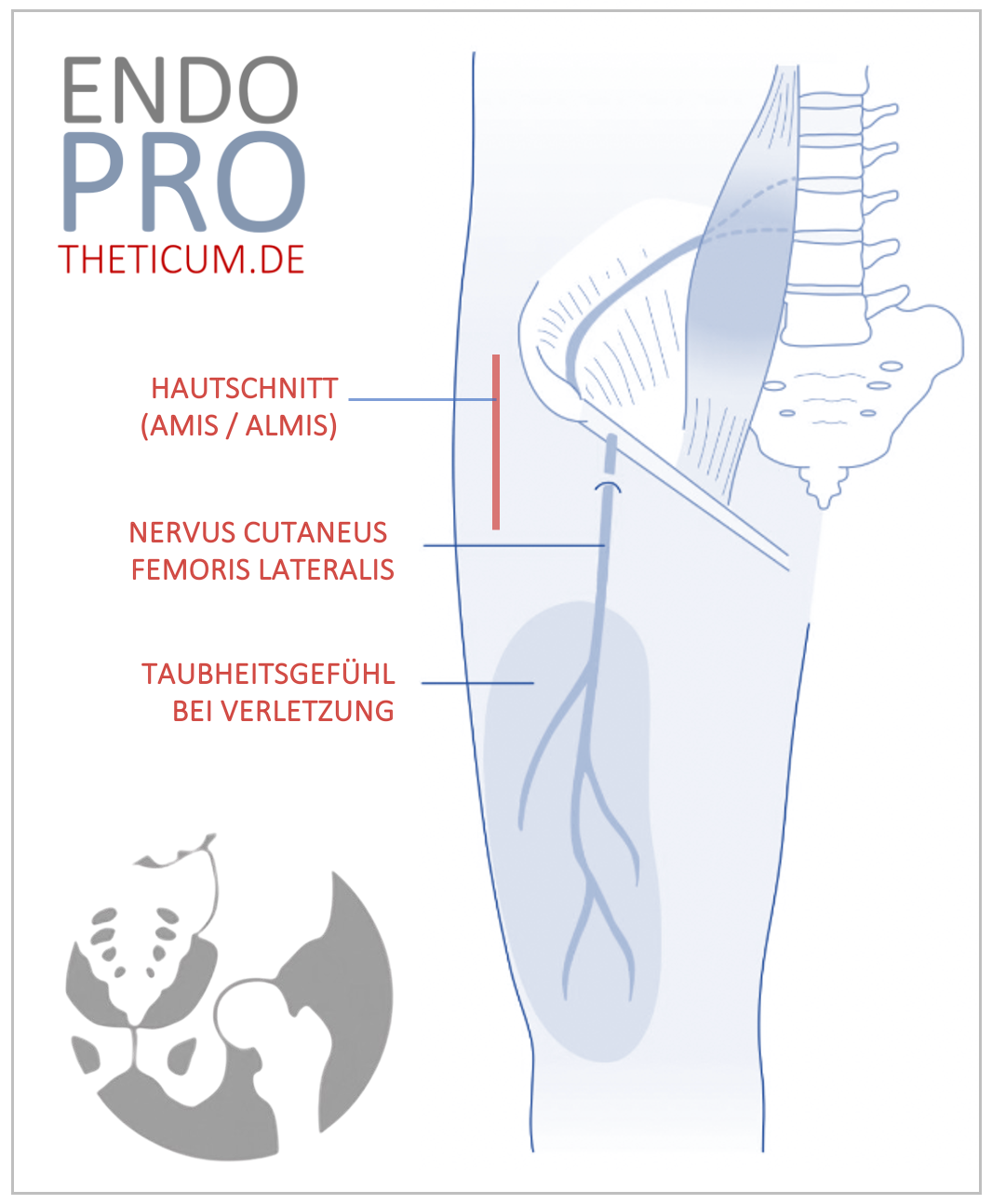
2. Surgical therapy
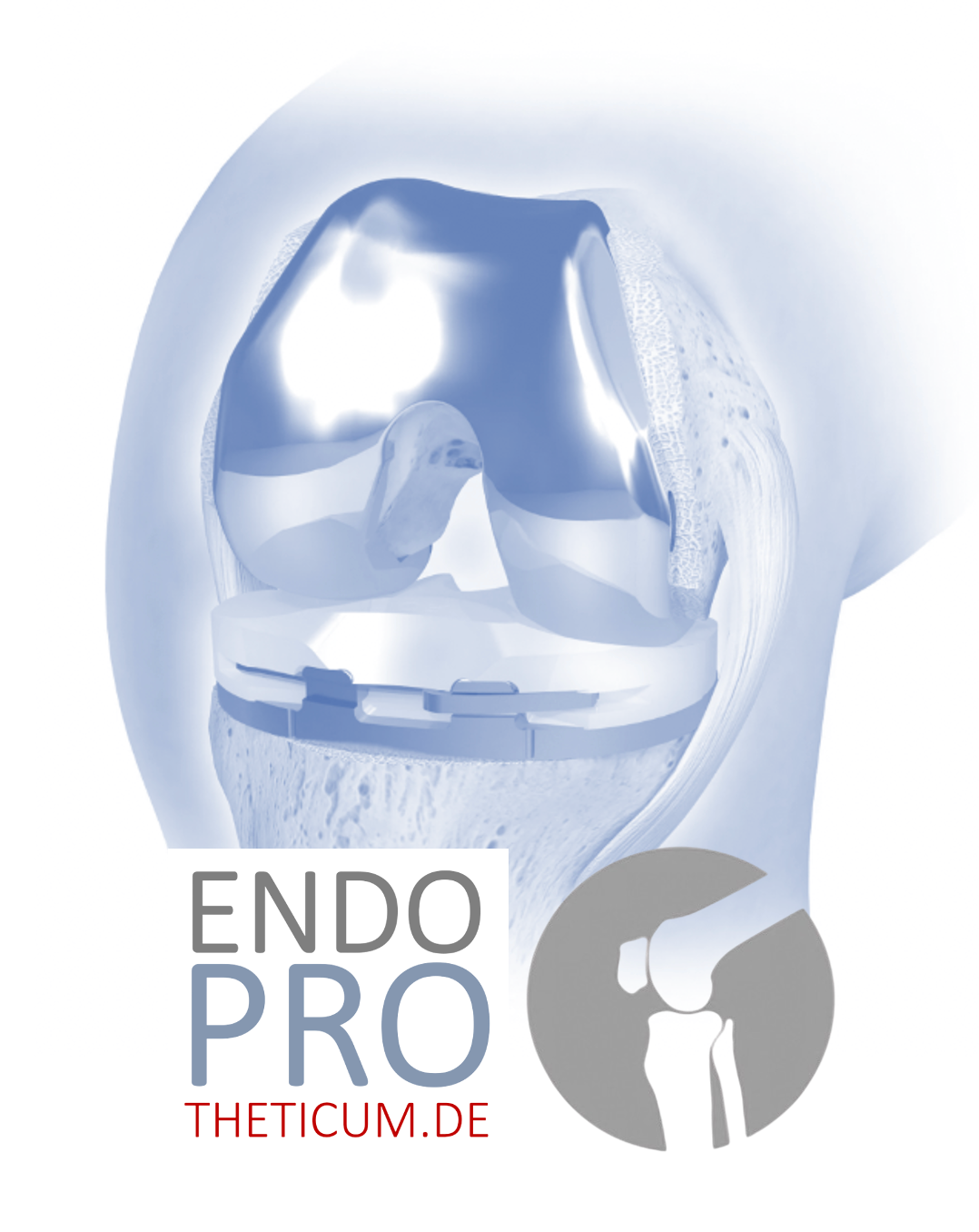
- Joint replacement: Hip prosthesis in cases of severe wear and tear.
- Minimally invasive procedures: Early intervention in cases of mild wear and tear.
Hip joint surgery for osteoarthritis
1. Indications for surgery
- Progressive pain.
- Severe restriction of movement.
2. Surgical methods
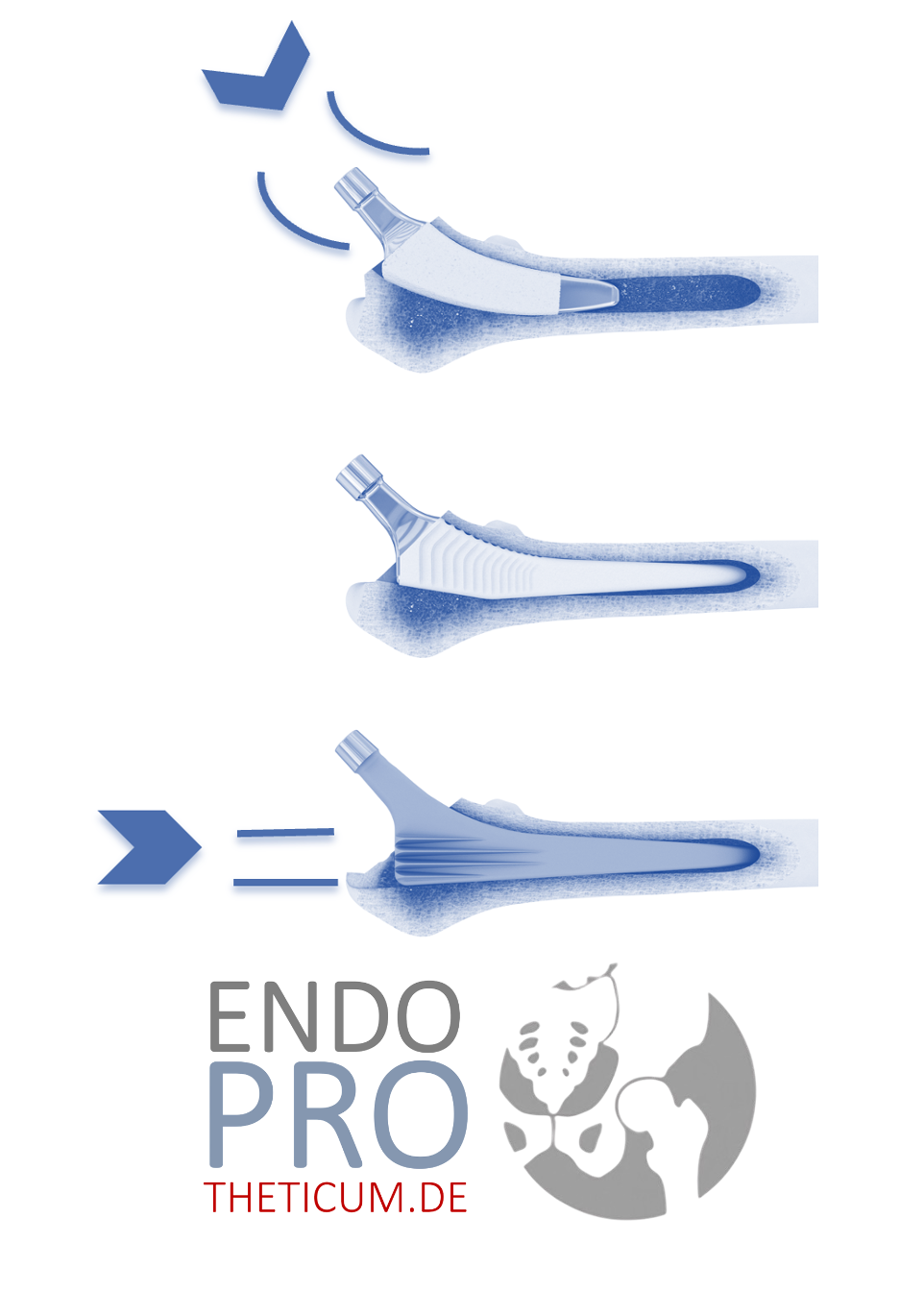
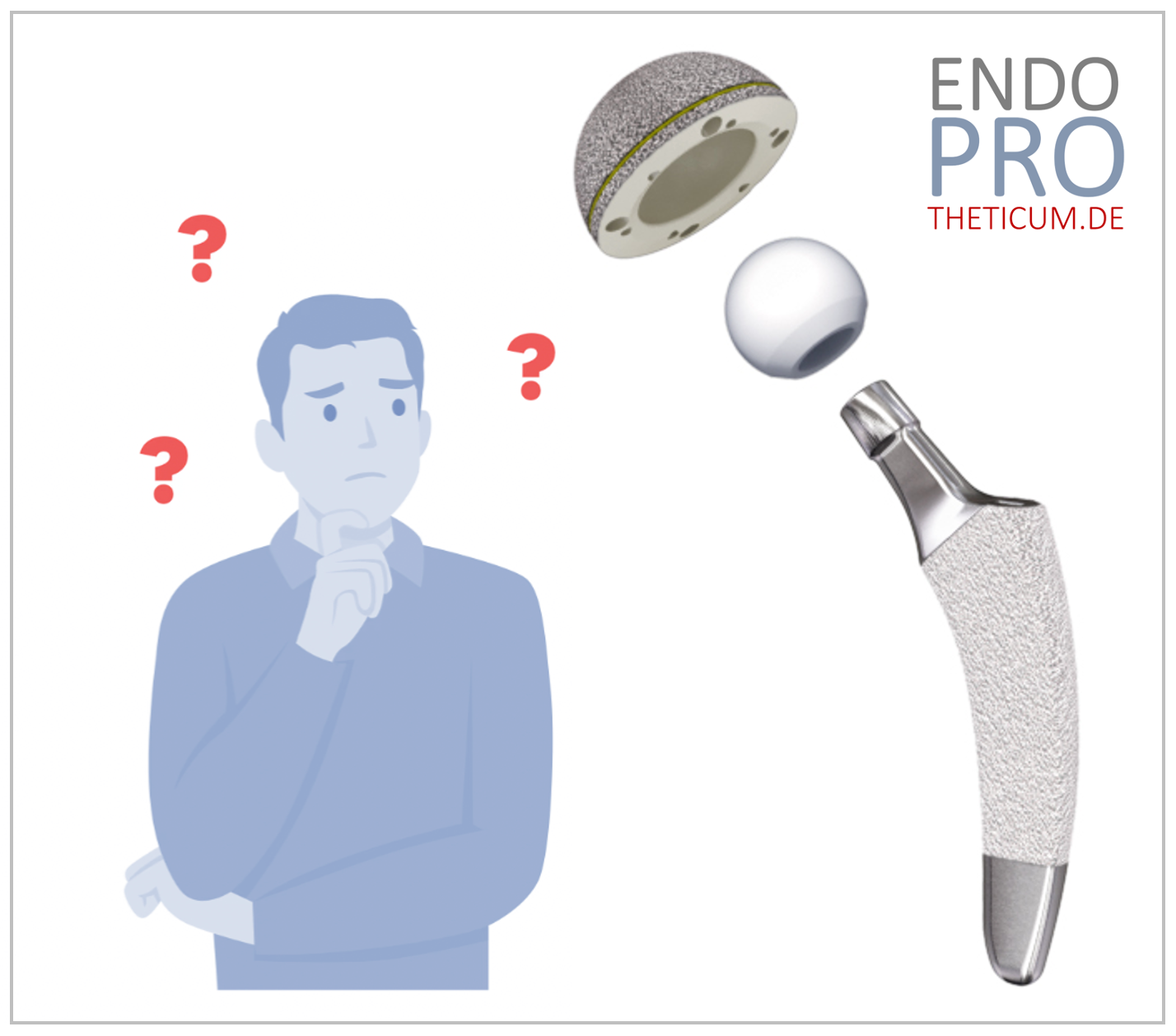
- Total endoprosthesis (TEP): Complete replacement.
- Short stem prosthesis: Suitable for younger patients.
3. Forecast and lifespan
- Durability of modern prostheses: currently expected to last 20-30 years.
Living with hip osteoarthritis
1. Everyday life simplifications
- Use of a walking stick or shoe lifts.
- Conversion of living space (accessibility).
2. Exercise and Sport
- Joint-friendly sports: swimming, cycling.
- Avoid high-impact sports such as jogging.
Prevention of osteoarthritis of the hip joint
1. Healthy lifestyle
- Weight control.
- A balanced diet with anti-inflammatory foods (e.g., fish oil, turmeric).
2. Correct load
- Regular moderate exercise to strengthen cartilage.
- Avoiding overload from heavy work.
Advances in osteoarthritis therapy
1. Biological therapy approaches
- Use of stem cells.
- Gene therapy for regeneration.
2. Future technologies
- 3D-printed implants.
- Robot-assisted surgeries.
Frequently asked questions about osteoarthritis of the hip
How quickly does hip osteoarthritis progress?
The progression of osteoarthritis in the hip joint varies greatly from person to person. Factors such as overall joint stress, genetic predisposition, and body weight play a crucial role. Often, the disease begins with mild symptoms that can worsen over the years. However, early diagnosis and the initiation of appropriate therapy can help slow the progression of osteoarthritis and maintain quality of life.
Can osteoarthritis of the hip joint be cured?
Currently, there is no cure for osteoarthritis, as the cartilage damage is irreversible. However, conservative or surgical therapies can reduce pain and improve mobility. The goal is to control symptoms and slow the progression of the disease as much as possible.
Which sports are suitable for people with osteoarthritis of the hip?
Gentle forms of exercise such as swimming, cycling, or Nordic walking are recommended for hip osteoarthritis. These activities promote blood circulation, support cartilage nutrition, and strengthen muscles without putting excessive strain on the joints. High-impact sports such as running or football, on the other hand, should be avoided.
When should a hip replacement be considered?
A hip replacement is generally recommended when conservative therapies are no longer sufficient to relieve pain or maintain mobility. If quality of life is severely impaired and daily activities such as walking, standing, or climbing stairs become challenging, a total hip replacement (THR) can be an effective solution.
What are the latest advances in the treatment of osteoarthritis?
Modern medicine is constantly developing new approaches to treating osteoarthritis. These include:
- Biological therapies: Use of stem cells for cartilage regeneration.
- Advanced implants: Custom-made prostheses for better adaptation to individual anatomy.
- Digitalization: Applications and wearables to improve therapy monitoring and adjustment.
- Minimally invasive surgical techniques: Gentler procedures with shorter recovery times and a lower risk of complications.
How long does a hip replacement last in cases of osteoarthritis?
The lifespan of a hip replacement used to be typically 15 to 20 years. Today, a lifespan of 20 to 30 years is more realistic. This period can be shorter in younger patients or those with strenuous physical activity. However, thanks to modern materials and techniques, prostheses with longer lifespans are also available. Regular follow-up examinations are crucial for the early detection of any potential complications.
What alternatives are there to surgery for osteoarthritis?
In addition to surgical treatment, the following options are available:
- Injections of hyaluronic acid or platelet-rich plasma (PRP).
- Physiotherapy to strengthen muscles and improve mobility.
- Painkillers and anti-inflammatory drugs.
The choice of therapy depends on the severity of the osteoarthritis, the patient's age, and their overall health. A comprehensive consultation with a specialized orthopedic surgeon is recommended.
Conclusion
Osteoarthritis of the hip (coxarthrosis) is a challenge that can be both physically and psychologically taxing for those affected. Nevertheless, there are numerous ways to maintain quality of life and slow the progression of the disease. With the right therapeutic approaches and early diagnosis, patients can lead an active and fulfilling life. Developments in joint replacement and biological medicine offer hope for increasingly better treatment options in the future.
MAKE AN APPOINTMENT?
You are welcome to make an appointment either by phone or online .