Meniscus tear: traumatic or degenerative?
Degenerative meniscus tear due to wear and tear:
Why arthroscopy (knee arthroscopy) often doesn't help

Why the difference in meniscus tears is crucial
The meniscus acts as a shock absorber and stabilizer in the knee, which is why its integrity is essential for the joint's functionality. A meniscus tear (meniscal lesion) in the knee is one of the most common knee injuries – but not all tears are the same. The crucial difference lies in whether the tear resulted from a sudden trauma or whether it develops degeneratively over years of wear and tear, often as part of early-stage osteoarthritis. This distinction is important not only for diagnosis but, above all, for choosing the right treatment.
An acute, traumatic meniscus tear in a young athlete must be treated very differently than a tear caused by wear and tear in an older person.
This comprehensive article examines in detail the differences between traumatic and degenerative meniscal injuries. It discusses the mechanisms of injury, affected groups, symptoms, and corresponding treatment options. Furthermore, it explores why arthroscopy is often ineffective in cases of wear-related meniscal lesions, such as those caused by osteoarthritis, and what alternatives, such as unicompartmental knee replacement, are available. Finally, the negative consequences of partial meniscectomy, a procedure frequently performed during arthroscopy, are addressed.
The meniscus – anatomy and function in the knee joint
The meniscus is a crescent-shaped cartilage disc in the knee joint. There are two menisci in each knee:
- Medial meniscus : It is less mobile and therefore tears more frequently.
- Outer meniscus : More flexible and less frequently affected by tears.
The main functions of the meniscus:
- Shock absorber: It distributes the body weight evenly across the articular cartilage.
- Stabilization: The meniscus provides greater stability, especially during rotational movements.
- Joint protection: It protects the cartilage and prevents premature wear.
A torn meniscus significantly disrupts these functions – and depending on the cause, this can have different consequences.
Traumatic meniscus tear – cause of accident and typical symptoms
A traumatic meniscus tear usually occurs due to a sudden, abrupt movement of the knee – often during sports such as soccer, skiing, or tennis. Classic movements that lead to a tear include:
- Knee twisting with the foot fixed
- Sudden changes of direction
- Hyperextension or flexion with high force
🔹 Typical symptoms of a traumatic meniscus tear:
- Acute, stabbing pain in the knee
- Swelling within hours
- A feeling of blockage (the knee "sticks")
- Grinding or snapping in the knee
- Limited mobility
Those affected are mostly young, active people and athletes.
👉 Diagnosis: To assess a meniscus tear, a clinical examination (e.g., McMurray test) is performed. For a definitive diagnosis, an MRI (magnetic resonance imaging) scan is the gold standard.
Degenerative meniscus tear – wear and tear and osteoarthritis as triggers
A degenerative meniscus tear develops due to gradual wear and tear. The tissue becomes brittle over the years and eventually tears, often even during everyday movements.
🔹 Who is affected?
- Older people (aged 50 and over)
- Patients with existing osteoarthritis
- overweight people
- People with deformities (e.g. bowlegs)
🔹 Typical symptoms of a degenerative meniscus tear:
- Pain on the inside of the knee
- Start-up pain after periods of rest
- Pain when climbing stairs or squatting
- Often no acute trauma is present in the background
👉 Diagnosis: Here too, MRI is the method of choice to visualize the tear and accompanying cartilage damage.
Diagnosis of a meniscus tear
Precise diagnosis is crucial to distinguish between a traumatic and a degenerative meniscus tear. Several examination methods are used for this purpose:
Medical history (patient interview)
The doctor asks the patient detailed questions about:
- Complaints : How long have you been experiencing pain? Was there a specific accident or did the symptoms develop gradually?
- Pain location : Internal or external pain, dependent on exertion or constant?
- Accompanying symptoms : feeling of instability, blockages, cracking noises?
- General medical history : Previous knee injuries, existing osteoarthritis, occupational or sporting stresses?
👉 Important:
- Acute trauma and sudden pain indicate a traumatic meniscus tear.
- Gradual pain without a clear cause is more indicative of degenerative changes .
Clinical examination
The doctor checks the knee joint for:
- Swelling (joint effusion)
- Mobility (extension and flexion limitations)
- Pressure pain along the joint line
In addition, targeted meniscus tests are used:
- McMurray test
The doctor rotates the lower leg inwards and outwards with the knee bent. Pain or an audible "click" suggests a meniscus tear.
- Apley grinding test
The patient lies prone with the knee bent at a right angle. The doctor presses down on the shinbone and rotates it. Pain indicates a meniscus tear.
- Steinmann I and II tests
By actively and passively rotating the lower leg inwards and outwards, the doctor checks whether pain occurs at the joint space.
👉
Note:
Tests are often less conclusive in cases of degenerative cracks. Imaging is particularly important in these cases.
Diagnostic imaging
X-ray image
Although X-rays do not show meniscus injuries themselves, they help accompanying changes , e.g.:
- Joint space narrowing (indication of osteoarthritis)
- Osteophytes (bone growths caused by wear and tear)
- Axial misalignments (X- or O-legs)
👉 Important: If a purely traumatic meniscus injury without osteoarthritis is suspected, the X-ray image is usually unremarkable.
Magnetic resonance imaging (MRI)
MRI is considered the gold standard for diagnosing meniscus tears. It shows in detail:
- Location and extent of the crack
- Cartilage condition
- joint effusion
- Associated injuries (e.g. cruciate ligament tears)
👉 Differences in the MRI image:
- Traumatic meniscus tear : Usually a clear, localized tear pattern.
- Degenerative meniscus tear : Fringe-like, diffuse lightening in the meniscus tissue.
Ultrasound (sonography)
Ultrasound is suitable for quickly assessing joint effusion or major meniscus changes . However, it is not as precise as an MRI.
Treatment of meniscus tears: Which therapy is suitable for which tear?
The therapy depends on the type of tear, the patient's age, accompanying injuries, and activity level.
🔹 Traumatic meniscus tear:
- Conservative treatment: For small, stable tears – physiotherapy and pain therapy
- Arthroscopy with sutures: For fresh tears in well-vascularized areas
- Partial resection: Removal of damaged tissue (only if suturing is not possible)
🔹 Degenerative meniscus tear:
- Conservative therapy: pain medication, weight reduction, physiotherapy
- Arthroscopy? Usually not useful, as the underlying cause (wear and tear) remains.
- Alternative: Unicompartmental knee replacement for advanced osteoarthritis
Conservative treatment of a meniscus tear (without surgery)
Especially in the case of small, stable traumatic meniscus tears and degenerative meniscus lesions conservative treatment is often the first choice.
Goals of conservative therapy:
- Pain relief
- Reduction of swelling
- Restoration of mobility
- Building up the stabilizing muscles
👉 Overview of conservative measures:
- Rest: Temporary relief and adjustment of activity (e.g., avoiding twisting movements).
- Cooling: Ice packs to reduce swelling (15-20 minutes each, several times a day).
- Elevation: Supports the reduction of swelling.
- Medications: Painkillers (e.g., ibuprofen or diclofenac) have a pain-relieving and anti-inflammatory effect.
- Physiotherapy: Targeted exercises strengthen the muscles, stabilize the joint and improve mobility.
- Injections: Hyaluronic acid (for incipient osteoarthritis) or cortisone (for acute inflammation) can alleviate symptoms.
👉 When conservative therapy is appropriate:
- Degenerative meniscus tear without blockage or instability
- Small traumatic tears without entrapment
- Simultaneous osteoarthritis (especially in people over 50)
Types of surgery for meniscus tears
Depending on the type and location of the meniscus tear, different procedures are possible:
a) Meniscus suture (meniscus reconstruction)
Fresh, traumatic tears in the well-vascularized outer zone of the meniscus can be sutured.
Advantages:
- Preservation of the meniscus (important for long-term joint stability)
- Reduced risk of developing osteoarthritis later in life
Disadvantages:
- Longer rehabilitation period (3-6 months of relief needed)
- Suture healing is not always successful
👉 Suitable for:
- Young, active patients
- Fresh traumatic tears in the vascularized area
b) Partial meniscectomy (partial removal)
In the case of tears in the non-vascularized zone (white zone) or severely damaged tissue, the damaged part is removed and the meniscus is smoothed.
Advantages:
- Rapid recovery (rehab often only 2-6 weeks)
- Pain relief usually occurs quickly
Disadvantages:
- Reduced buffering function → Higher risk of osteoarthritis
- Instability is possible, especially with larger resections
👉 Suitable for:
- Traumatic tears that cannot be stitched
- Acute blockages
c) Meniscus transplantation
In cases of complete meniscus removal (e.g., after previous resection) and persistent symptoms, a donor meniscus be transplanted.
👉 This is rarely done , especially in young patients without osteoarthritis.
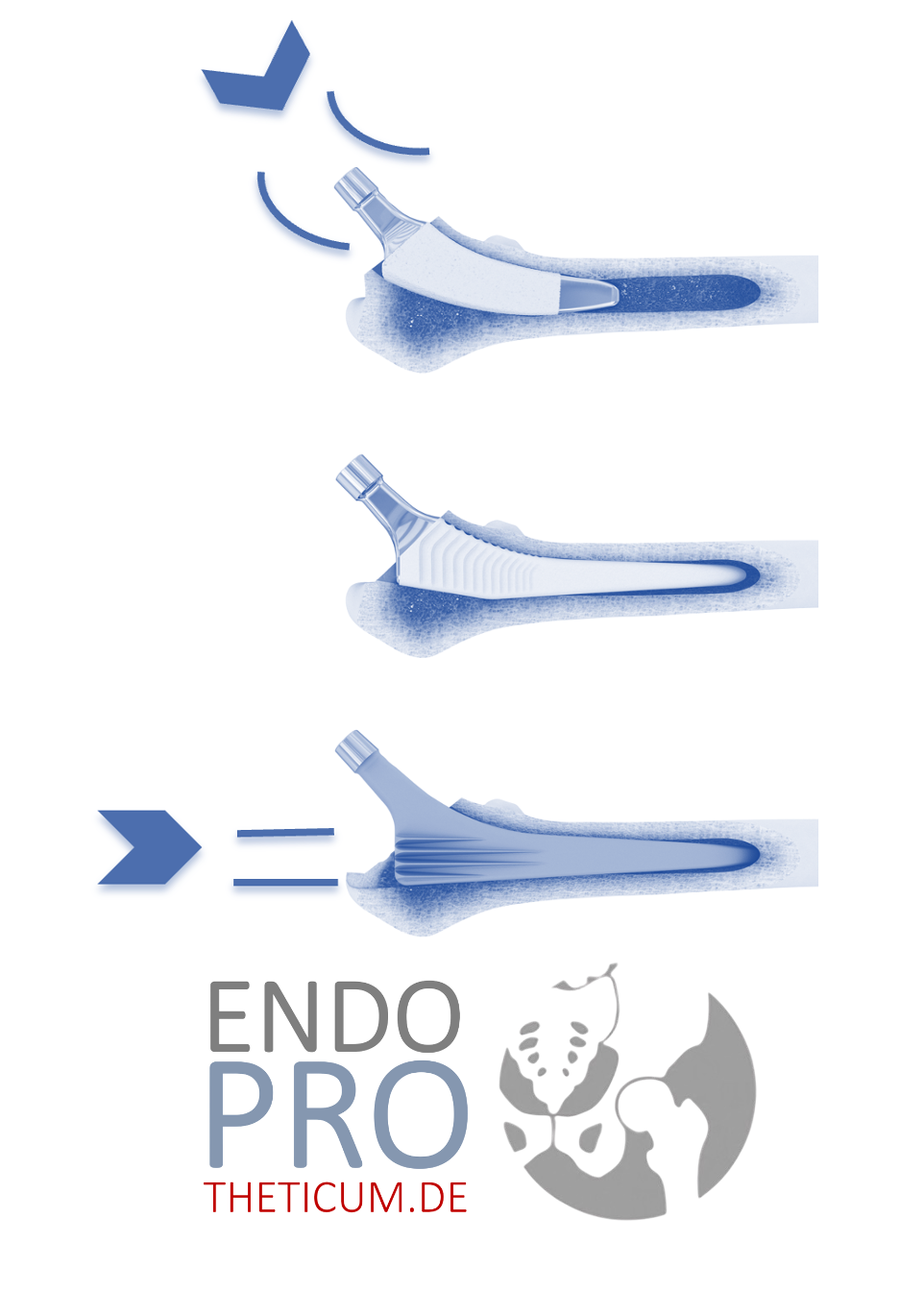
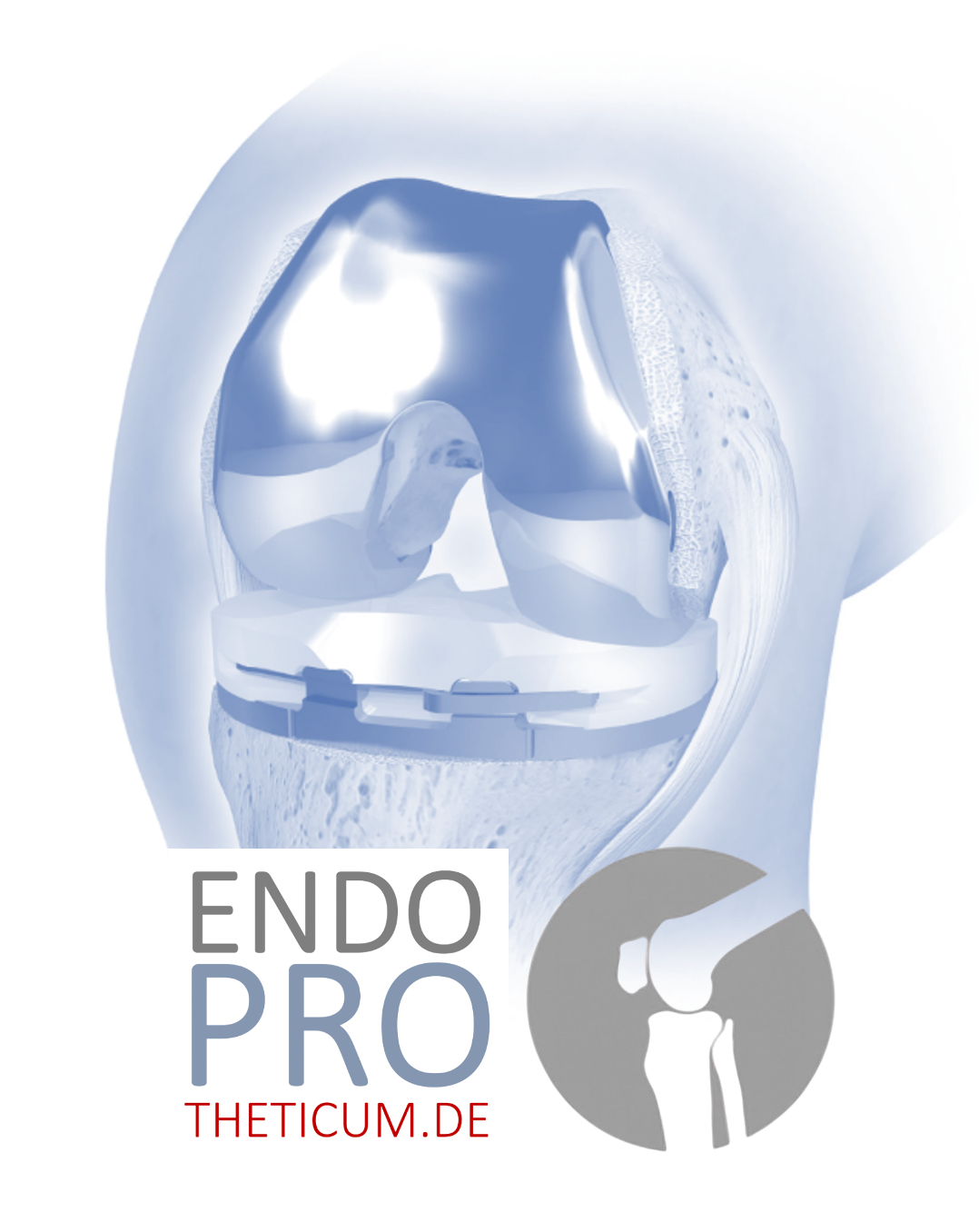
Alternative: Unicompartmental joint replacement (partial joint replacement)
In cases of degenerative meniscus tears with existing osteoarthritis, arthroscopy often does not bring long-term success — in these cases, a partial knee replacement be a sensible option.
What is a sled prosthesis?
It only replaces the worn part of the joint (usually the inner knee compartment) and preserves the healthy parts .
👉 Advantages:
- Less bone loss than with a full prosthesis
- Natural movement sensation is preserved
- Shorter rehabilitation than with a total endoprosthesis
👉 Suitable for:
- Patients with unilateral cartilage wear
- Well-preserved remaining joint
Unicompartmental knee replacement as a solution for degenerative meniscus tears and osteoarthritis
A partial knee replacement only replaces the damaged part of the knee joint – usually the inner part. Advantages:
- Preserving a healthy knee
- Faster rehabilitation
- More natural feeling of movement
- Longer lifespan than complete dentures when indicated correctly
Consequences and risks of a partial meniscectomy – why the knee becomes unstable
Many people think: "If the damaged part is gone, the pain will also be gone." Unfortunately, partial resection often leads to instability because the meniscus is missing as a stabilizer.
🔹 Consequences:
- Higher risk of osteoarthritis
- Faster cartilage wear
- Persistent pain
Long-term prognosis after meniscus surgery
🔹 Meniscus suture:
- Good results in younger patients and fresh, traumatic tears in well-vascularized areas.
- Healing rate: 60-80% (depending on the type and location of the tear).
- Long-term prognosis: If the healing process is successful, the knee remains stable and the risk of osteoarthritis is lower than after a partial resection.
🔹 Partial removal (resection):
- Rapid pain reduction , but:
- The meniscus loses its buffering and stabilizing function.
- The risk of cartilage damage and osteoarthritis increases because the load is no longer distributed evenly.
- Long-term prognosis: Mixed , depending on the size of the removed meniscus fragments. Osteoarthritis often develops earlier .
🔹 Sled prosthesis:
- Often the best option for advanced osteoarthritis and degenerative meniscus damage.
- Good durability: 15-20 years with appropriate load control.
- Prognosis: Very good for localized joint wear – better mobility and less pain compared to total joint replacement.
Conclusion: The right therapy for the right meniscus tear
Not all meniscus tears are the same. While a traumatic tear can often be successfully treated arthroscopically, a more cautious approach to surgery is recommended for degenerative tears. Especially in cases of advanced osteoarthritis, a partial knee replacement may be the better option to restore mobility and quality of life.
For patients with significant osteoarthritis or advanced cartilage wear, a unicompartmental knee replacement the more functional and sustainable solution, as it replaces the damaged part of the knee joint without sacrificing the entire joint.
👉 Do you have knee problems and don't know which treatment is best?
Consult an experienced knee specialist!
MAKE AN APPOINTMENT?
You are welcome to make an appointment either by phone or online .