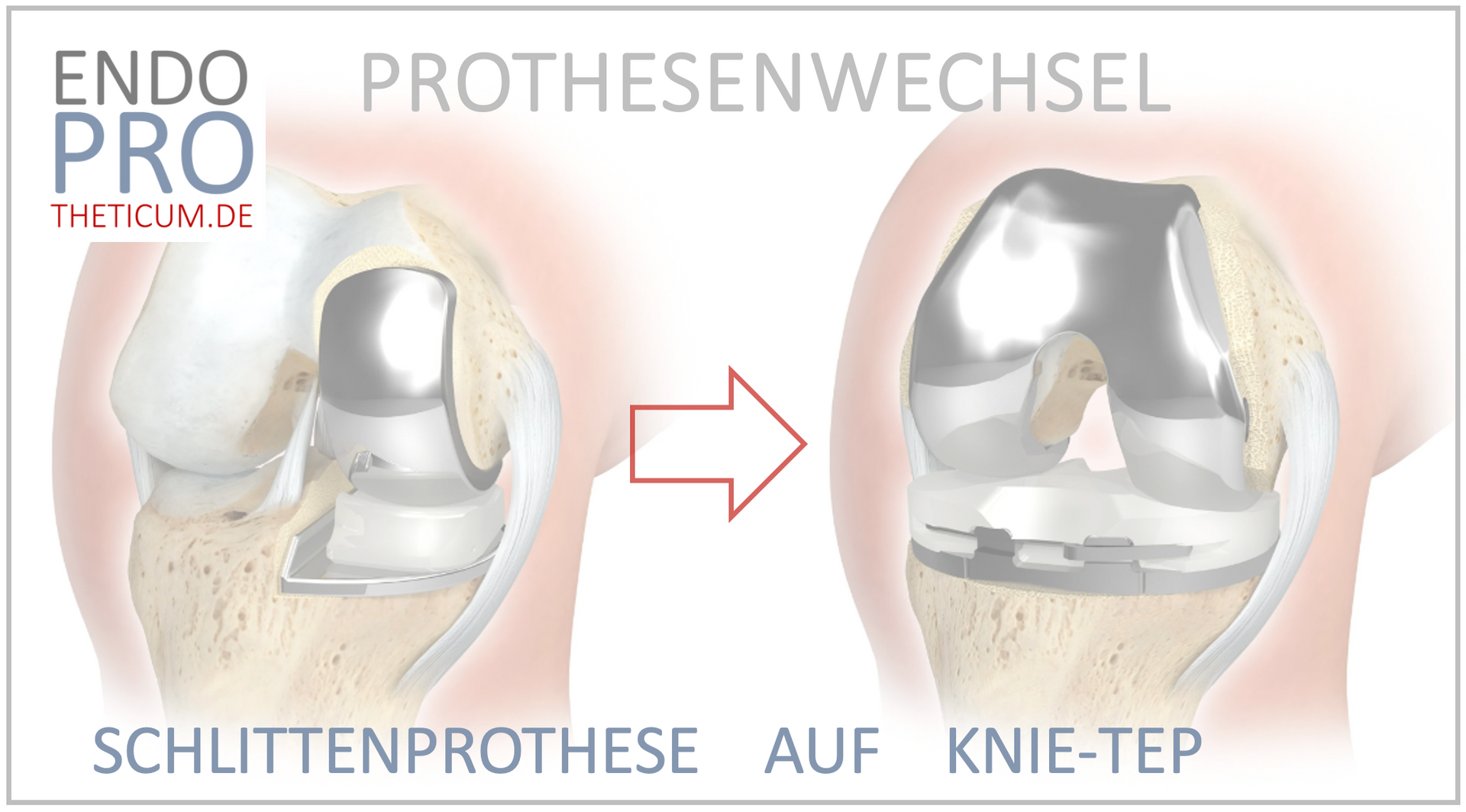
When the partial knee replacement fails: Everything you need to know about switching to a total knee replacement
If a partial knee replacement is no longer sufficient, switching to a total knee replacement (TKR) is usually possible without any problems!
The partial knee replacement, often a preferred solution for patients with limited cartilage wear in the knee, offers many patients improved quality of life and mobility. However, like all implants, the partial knee replacement has its limitations. If it fails, a total knee replacement (TKR) becomes necessary. This blog explains when and why such a revision is required, what options are available, and why modern surgical techniques make these procedures safe and effective.
A common reason for revision of a partial knee replacement is the spread of osteoarthritis to other parts of the knee joint that were healthy during the original surgery. Fortunately, in most cases, the conversion from a partial knee replacement to a total knee replacement is a well-planned and complication-free procedure.
In this comprehensive blog, we take a detailed look at the background of a knee replacement revision. We explain the most common causes and modern treatment approaches. Whether you are personally affected or simply want to learn more – here you will find all the answers you need about knee replacement surgery.
Reasons for switching from a partial knee replacement to a total knee replacement
A change from a partial knee replacement to a total knee replacement (TKR) becomes necessary when the original prosthesis no longer fulfills its function. The main reasons for this can be divided into four categories:
- Progressive osteoarthritis:
Originally, partial knee replacement was intended to limit the damage to a specific area of the knee joint. However, in many cases, cartilage loss progresses over time and affects other joint areas, particularly the cartilage behind the kneecap (retropatellar). In such cases, a partial replacement is no longer sufficient, and a total knee replacement becomes necessary. - Loosening and wear:
Although modern partial knee replacements are durable, they can loosen or wear out over the years. This is often due to overuse or age-related changes in bone density, which compromise the stability of the prosthesis. - Infections:
A periprosthetic infection is one of the most feared complications after knee surgery. Although rare, it can necessitate removal of the partial knee replacement and conversion to a total knee replacement. - Instability:
If the knee does not feel stable enough after implantation or exhibits repeated failures, this is a clear indication that revision surgery is necessary. In these cases, a total knee replacement (TKR) offers more comprehensive support and greater stability.
Signs of a partial knee replacement failure
A partial knee replacement initially allows for a high degree of mobility and functionality, but problems can arise over the years. There are clear signs that the prosthesis is no longer performing its function optimally.
- Increasing pain: If pain occurs that persists even at rest or during light activity, this is a warning sign. Particularly distressing are dull, persistent knee pain or sharp pain during exertion.
- Limitations in daily life: Those affected often report difficulties walking, climbing stairs, or performing other everyday movements. Swelling in the knee can also indicate a malfunction.
- Knee instability: A feeling that the knee is "giving way" or is wobbly indicates mechanical problems with the prosthesis. This is often associated with reduced confidence in the stability of the leg.
- Radiological changes: Imaging procedures such as X-rays or MRI often show early signs of loosening, wear and tear or mispositioning of the prosthesis.
Early medical evaluation of these symptoms can prevent the symptoms from worsening and a more comprehensive revision from becoming necessary.
Diagnostics before prosthesis replacement
Before a revision from partial knee replacement to total knee replacement is performed, a precise diagnosis is required. Physicians use a combination of medical history, clinical examination, and state-of-the-art diagnostic procedures to determine the need for revision.
- Medical history: Patients are specifically asked about their complaints, e.g. type and intensity of pain, time of onset and limitations in everyday life.
- Clinical examination: Orthopedists check the mobility, stability, and alignment of the knee. Swelling, redness, or warmth in the area of the prosthesis may indicate inflammation.
- Imaging:
- X-ray: Shows mechanical changes such as loosening or misalignment.
- MRI: Provides detailed images of soft tissues and helps identify inflammation or progressive osteoarthritis.
- Scintigraphy: Used to detect infections or bone remodeling activity.
- Laboratory tests: Blood tests for infection markers such as CRP or leukocyte count are essential to rule out an infection.
This comprehensive diagnosis lays the foundation for planning the revision and helps to tailor the appropriate therapy to the individual patient.
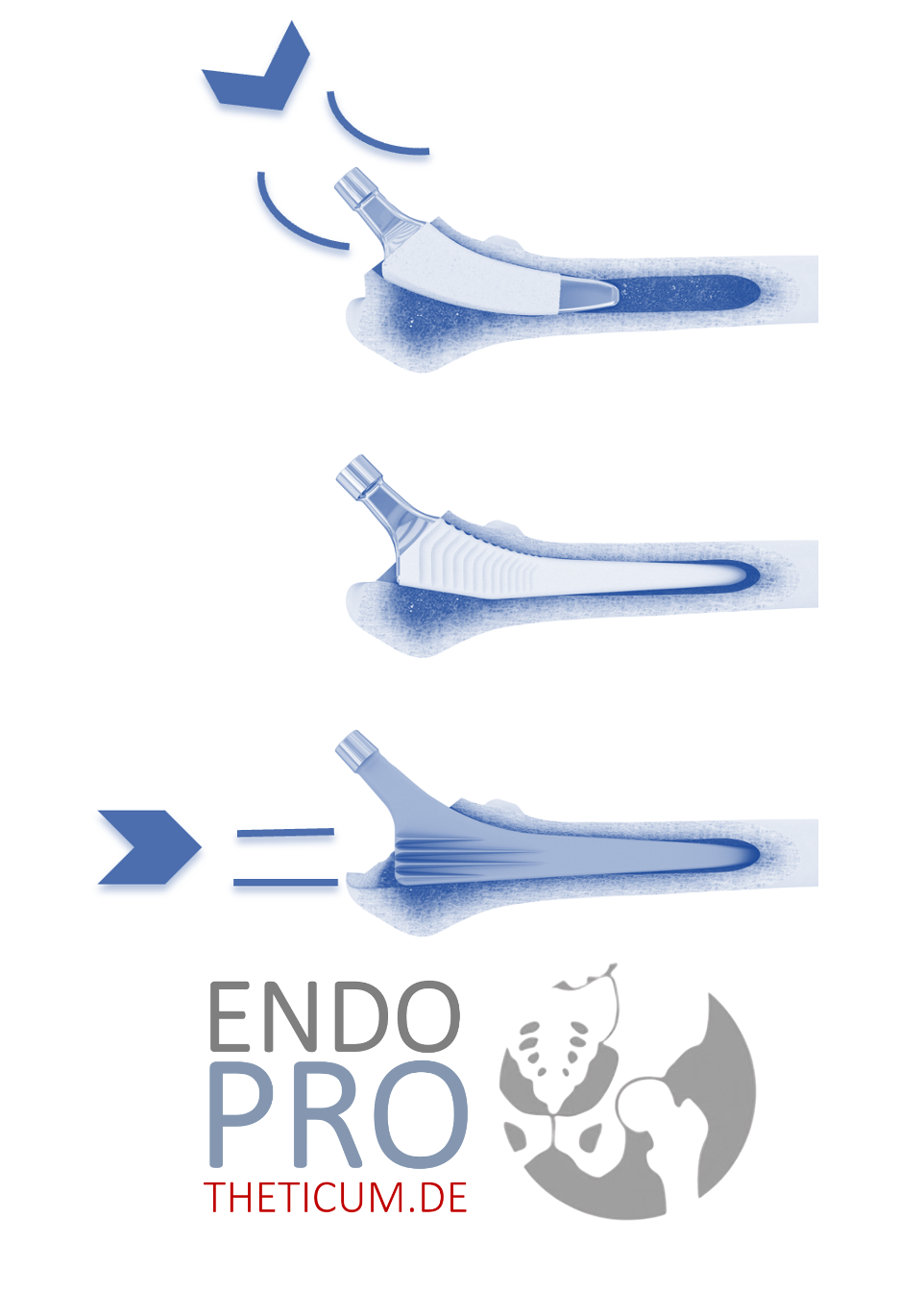
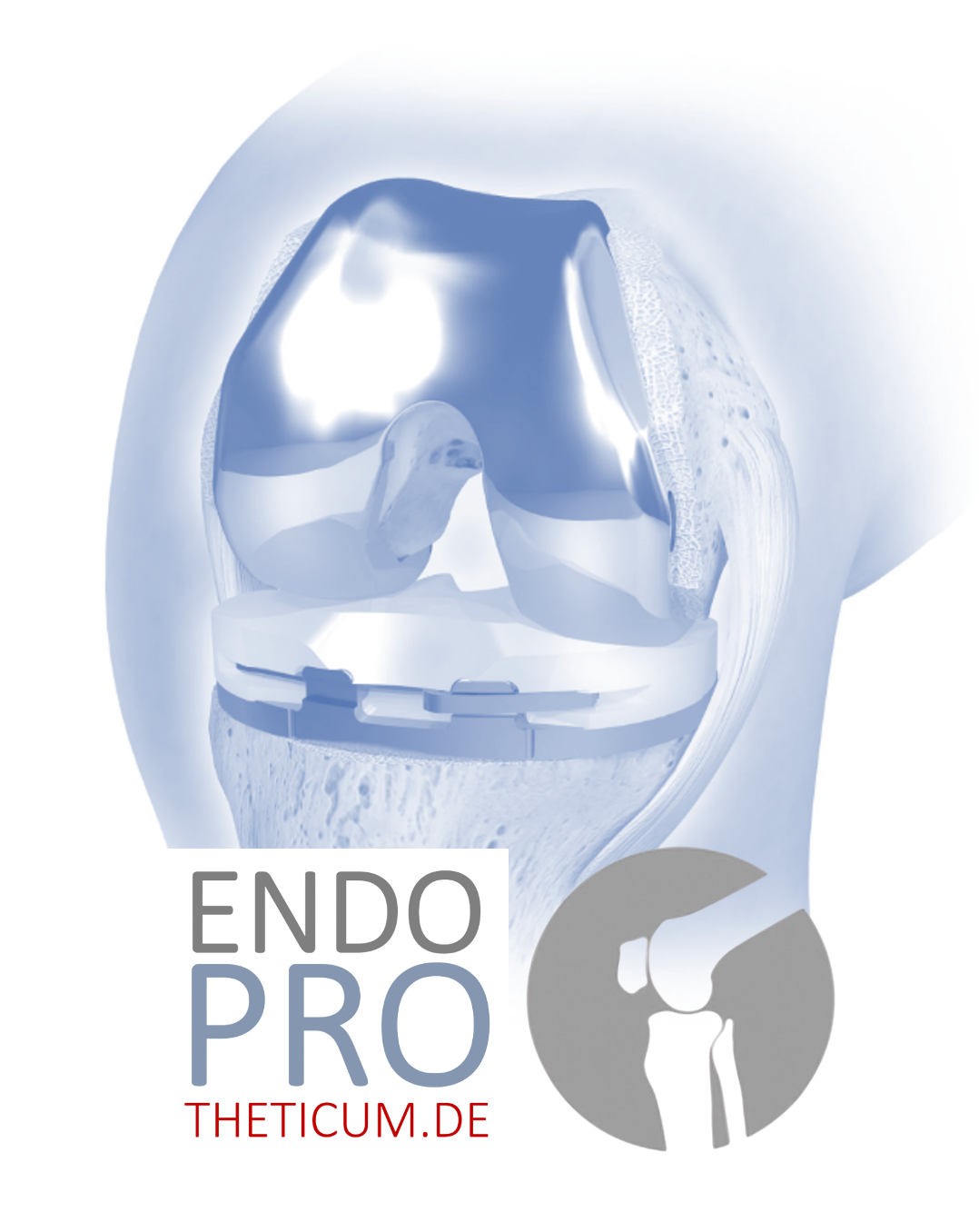
Prosthesis replacement: From partial knee replacement to total knee replacement
Switching from a partial knee replacement to a total knee replacement (TKR) is often the next step when the partial prosthesis no longer fulfills its function.
- Procedure for the revision: The procedure begins with the removal of the partial knee replacement. This is done with great care to protect the surrounding bone and soft tissue. The affected joint area is prepared, and the new total knee replacement is precisely fitted. Modern implants allow for optimal adaptation to the individual anatomy of the patient.
- Challenges: The greatest challenges lie in the precision required to preserve bone and to restore the biomechanics of the knee. However, experienced surgeons can overcome these hurdles using state-of-the-art technology.
- Minimally invasive approaches: By using gentle surgical methods, the strain on the body is reduced, which contributes to a faster recovery.
Thanks to advanced techniques, this procedure is usually easy to plan and has high success rates.
Aftercare and rehabilitation following prosthesis replacement
Follow-up care is crucial for a successful recovery and long-term stable knee function.
- Physiotherapy: Even in the first few days after surgery, patients begin guided exercises to mobilize and strengthen the muscles. The goal is to restore the natural mobility and function of the knee.
- Weight relief: For a few weeks, the use of crutches may be necessary to relieve the operated knee and give the implant time to fully integrate.
- Daily living assistance: Patients are instructed on how to safely manage everyday situations such as climbing stairs or lifting. Assistive devices such as occupational therapy can also be helpful.
- Regular check-ups: Follow-up appointments monitor the healing process. X-rays help to check the position and function of the implant.
A structured rehabilitation program makes a significant contribution to minimizing complications and quickly restoring quality of life.
Why switching is often possible without problems
Thanks to gentle surgical techniques and the experience of knee specialists, the conversion from a partial knee replacement to a total knee replacement goes smoothly in most cases.
- Bone preservation: When implanting a partial knee replacement, less bone is removed, which is advantageous in the event of a later revision.
- Modern implants: Knee replacements offer individual customization options, allowing them to easily integrate into the existing anatomy.
These factors make prosthesis replacement a safe and effective procedure today, with excellent long-term results.
Technical challenges when switching from partial knee replacement to total knee replacement
Converting from a partial knee replacement to a total knee replacement is a complex procedure, but thanks to modern surgical techniques and experienced surgeons, it can be performed safely. Some challenges include:
- Removal of the old prosthesis: Gently removing the unicompartmental prosthesis without further damage to the bone is crucial.
- Reconstruction of the anatomy: The surgeon must ensure that the new knee replacement fits exactly and that the natural joint geometry is restored as best as possible.
- Soft tissue injury: The operation potentially involves greater stress on soft tissues, especially if ligaments or structures have been weakened by the previous procedure.
- Precision of implantation: Misalignments must be avoided at all costs, as they could lead to premature wear and tear or new problems.
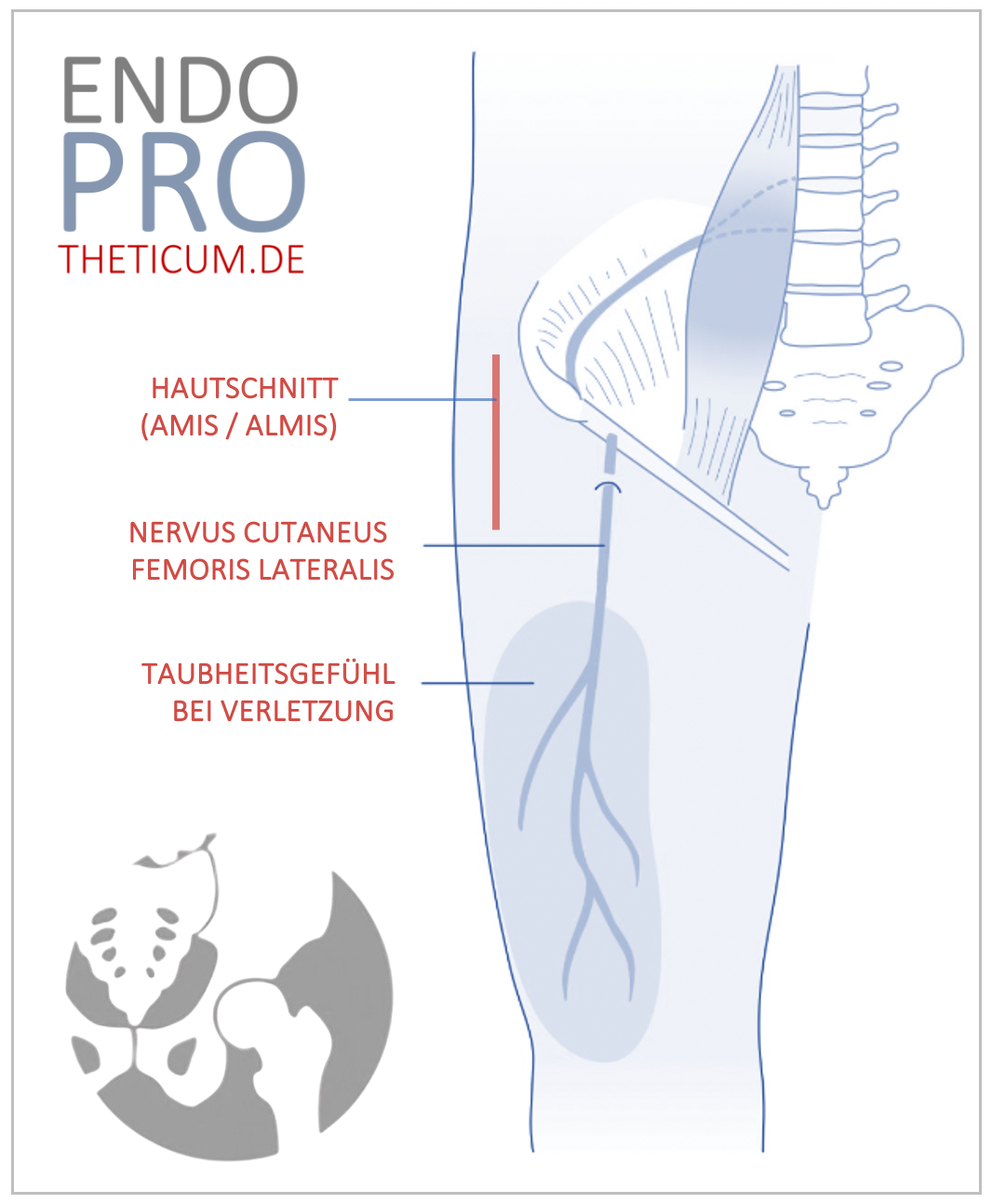
Modern surgical techniques for converting from partial knee replacement to total knee replacement
Minimally invasive surgery has made great strides in recent years, which has also significantly improved the transition from partial knee replacement to total knee replacement.
- Navigation and robotics: Modern techniques ensure maximum precision in positioning the new prosthesis. This improves long-term results and reduces the risk of complications.
- Bone preservation: Surgeons use minimally invasive approaches to preserve as much healthy bone substance as possible.
- Gentle soft tissue surgery: Reducing soft tissue damage decreases postoperative pain and promotes faster recovery.
- Access optimization: Optimized access minimizes scarring and reduces the risk of infection.
These advances make the switch significantly less stressful for patients today and increase the chances of success.
The role of rehabilitation after prosthesis replacement
After a conversion from a partial knee replacement to a total knee replacement, rehabilitation is a crucial factor for the long-term success of the surgery. Rehabilitation aims to restore strength, stability, and mobility in the operated knee and facilitate a return to daily life.
- Early mobilization: As early as the first or second day after surgery, patients begin gentle exercises under the guidance of a physiotherapist. This promotes blood circulation, reduces swelling, and supports healing.
- Targeted strengthening: Exercises to strengthen the thigh muscles and surrounding structures help to optimally stabilize the new joint.
- Gait analysis: Physiotherapists work with patients to restore a smooth gait pattern in order to avoid incorrect loading.
- Everyday-relevant exercises: Climbing stairs or walking on uneven terrain is also specifically practiced to increase safety in everyday life.
- Long-term physiotherapy: Even months after surgery, patients benefit from regular exercises to ensure full mobility and function of the joint.
An individualized rehabilitation program, tailored to the patient's needs and goals, maximizes the chances of recovery and quality of life.
Summary: The transition from partial knee replacement to total knee replacement
Switching from a partial knee replacement to a total knee replacement is often a necessary step when complications such as osteoarthritis progression or loosening occur. Thanks to modern surgical techniques and high-quality implants, this procedure is very successful in most cases.
Knee replacement surgery represents a comprehensive solution that not only reduces pain but also restores the stability and function of the knee joint in the long term. Supported by targeted rehabilitation and aftercare, patients can, in most cases, return to an active, pain-free life.
While switching from a partial knee replacement to a total knee replacement may seem intimidating at first glance, it is a routine procedure performed extremely safely in specialized centers by experienced knee surgeons. Thanks to state-of-the-art surgical techniques, high-quality implants, and optimized rehabilitation programs, patients today have excellent chances of permanently regaining their mobility and quality of life.
Specialized knee replacement centers possess a comprehensive understanding of the individual needs and challenges associated with revision surgery. They offer not only excellent surgical expertise but also patient-centered care that provides reassurance before, during, and after the operation.
Conclusion: Those who seek the help of a specialized expert early on benefit from precise diagnoses, tailored treatment strategies and the best chances for a complication-free recovery.
MAKE AN APPOINTMENT?
You are welcome to make an appointment either by phone or online .