Femoral head necrosis and total hip replacement: treatment options and chances of success
Treatment of femoral head necrosis using THA (hip prosthesis)

Femoral head necrosis, also known as avascular necrosis, is a serious disease in which the hip joint is damaged due to a lack of blood supply. This can lead to significant pain and restricted movement. A total hip arthroplasty (THA) is often the best solution to restore the quality of life of those affected. In this blog we will summarize the most important information about femoral head necrosis, the treatment options and the chances of success of a THA.
What is femoral head necrosis?
Femoral head necrosis, also known as avascular necrosis (AVN) or aseptic necrosis, is a condition in which the bone tissue in the femoral head dies due to insufficient blood supply. This can be caused by various factors such as trauma, certain medications (e.g. corticosteroids), alcohol abuse and medical conditions such as lupus erythematosus. The condition can occur at any age, but is more common in people between 30 and 50 years old.
Causes and risk factors of femoral head necrosis
The development of femoral head necrosis is multifactorial and can be triggered by a variety of causes and risk factors. The most important include:
- Traumatic causes:
- Fractures: Fractures in the area of the femoral neck or femoral head can damage the blood vessels that supply the femoral head, causing femoral head necrosis.
- Dislocations: Dislocations of the hip joint can affect the blood supply and lead to necrosis.
- Non-traumatic causes:
- Corticosteroid therapy: Long-term or high-dose use of corticosteroids can increase the risk of femoral head necrosis. The exact mechanism is not fully understood, but corticosteroids can promote fat accumulation in blood vessels and alter their permeability, which can lead to ischemia.
- Alcohol abuse: Chronic alcohol consumption can alter blood clotting and blood lipid levels, which can lead to damage to blood vessels and reduced blood flow to the femoral head.
- Certain diseases: Conditions such as lupus erythematosus, sickle cell anemia, and other systemic diseases may increase the risk of femoral head necrosis.
- Idiopathic causes:
- In many cases, the exact cause of femoral head necrosis remains unknown (idiopathic). It is thought that genetic factors and individual susceptibility may play a role.
Pathophysiology of femoral head necrosis
The pathophysiology of femoral head necrosis includes several stages:
- Ischemia:
- The impaired blood supply leads to ischemia, which means that the tissue does not receive sufficient oxygen and nutrients. This leads to the death of the bone cells (osteocytes).
- Bone loss and remodeling:
- After cell death, the body begins to break down the dead bone tissue and attempts to replace it with new bone tissue. However, this remodeling process is often inadequate, leading to weakening and instability of the femoral head.
- Collapse of the femoral head:
- Without adequate repair mechanisms, the weakened femoral head collapses under the weight and strain of the body. This leads to deformity and deterioration of joint function.
- Arthritis and joint destruction:
- Collapse of the femoral head leads to secondary osteoarthritis, a degenerative joint disease that causes pain, stiffness, and limited mobility. The joint surfaces become uneven and the cartilage wears away, further worsening symptoms.
Prevention and early detection of femoral head necrosis
Some measures and considerations are important for the prevention and early detection of femoral head necrosis:
- Regular medical checks: People with risk factors such as corticosteroid therapy or alcohol abuse should have regular medical checks to detect early changes in the hip joint.
- Early intervention: At the first sign of hip pain or restricted mobility, a doctor should be consulted immediately to enable early diagnosis and treatment.
- Healthy lifestyle: Avoiding excessive alcohol consumption and eating a balanced diet can reduce the risk of femoral head necrosis.
Femoral head necrosis is a serious condition that, if left untreated, can lead to serious complications. Early diagnosis and appropriate therapeutic measures, including the option of a total hip arthroplasty, can significantly improve the quality of life and mobility of those affected.
Symptoms and diagnosis of femoral head necrosis
The symptoms of femoral head necrosis often develop gradually and may initially go unnoticed. The most common symptoms include:
- Pain in the groin, thigh or buttocks
- Stiffness and limited mobility of the hip joint
- Pain that increases when walking or putting weight on the hip joint
Various imaging techniques are used to diagnose femoral head necrosis, including:
- X-rays
- Magnetic resonance imaging (MRI)
- Computed tomography (CT) These tests help determine the extent of damage and the stage of the disease.
Conservative treatment options for femoral head necrosis
In the early stages of femoral head necrosis, conservative treatment methods may be considered. These aim to relieve symptoms and slow the progression of the disease. Conservative treatment options include:
- Pain medication: Nonsteroidal anti-inflammatory drugs (NSAIDs) and other pain medications may be used to relieve pain.
- Physiotherapy: Exercises to strengthen the hip muscles and improve mobility.
- Stress reduction: Using walking aids such as crutches to relieve pressure on the hip joint.
- Lifestyle changes: reducing risk factors such as alcohol and tobacco consumption.
Surgical treatment options for femoral head necrosis
If conservative measures are not sufficient or the disease has already progressed, surgical interventions may be necessary. Common surgical procedures include:
- Coring: A minimally invasive procedure in which small holes are drilled into the femoral head to improve blood supply.
- Bone Grafting: Transplantation of bone tissue to stabilize the damaged area.
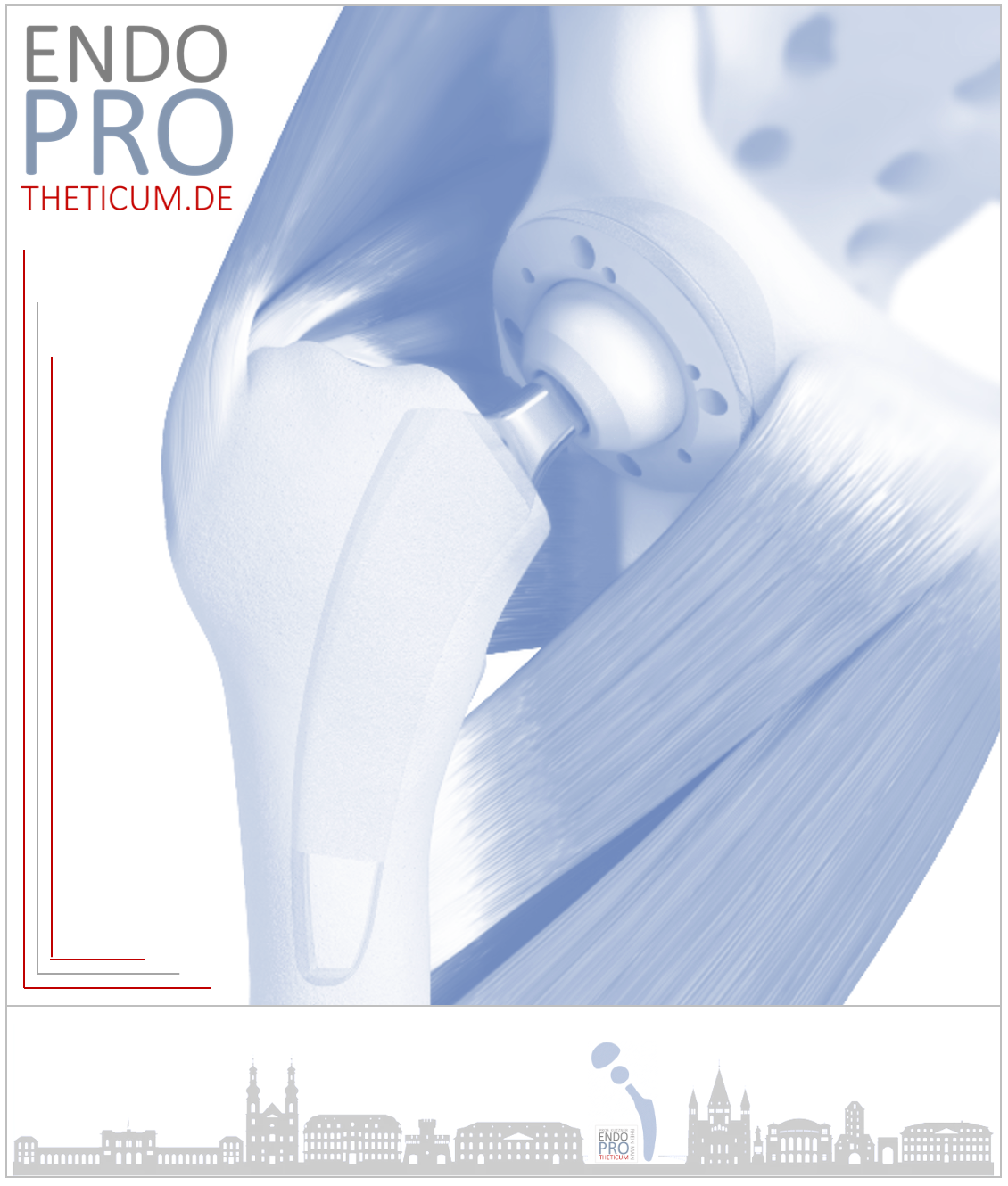
- Total hip endoprosthesis (THA): The complete replacement of the hip joint with an artificial joint. This method is often considered the best option for advanced femoral head necrosis.
THA: The path to freedom from pain in cases of femoral head necrosis
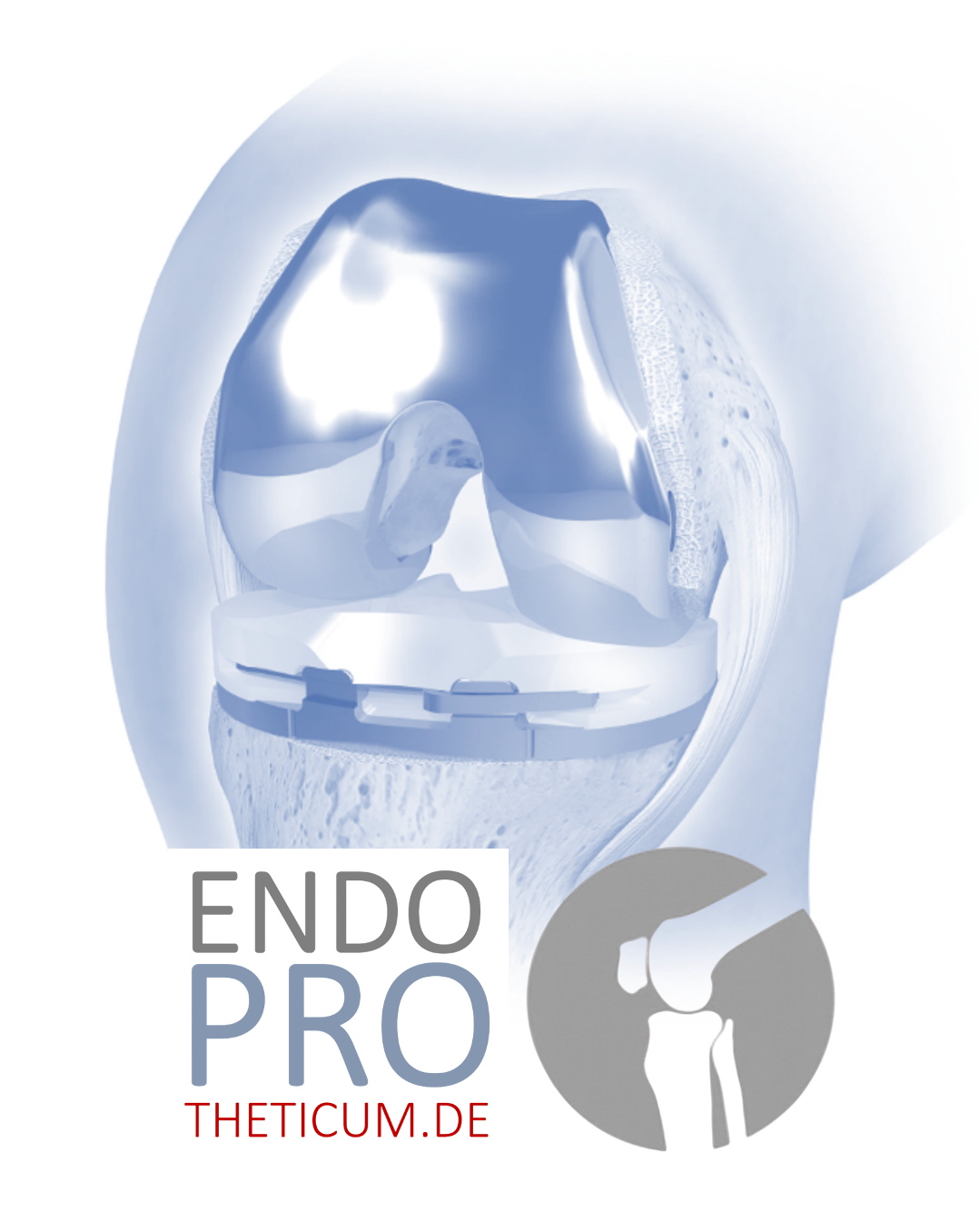
Total hip arthroplasty is a proven procedure for treating femoral head necrosis. The damaged hip joint is replaced with an artificial joint made of metal, plastic or ceramic. THA offers numerous advantages:
- Pain reduction: Most patients report significant pain relief after surgery.
- Improved mobility: The range of motion of the hip joint is significantly improved.
- Increased quality of life: Patients can lead a more active life again and carry out everyday activities without pain.
Preparation for total hip replacement
Preparing for a total hip replacement involves several steps to ensure the best possible treatment success:
- Preoperative examinations: To assess the patient's general health and identify any risk factors.
- Patient education: Information about the procedure of the operation, the postoperative measures and the expected results.
- Physiotherapy: Physiotherapeutic measures can be initiated before the operation to strengthen the muscles and promote recovery.
The surgical procedure
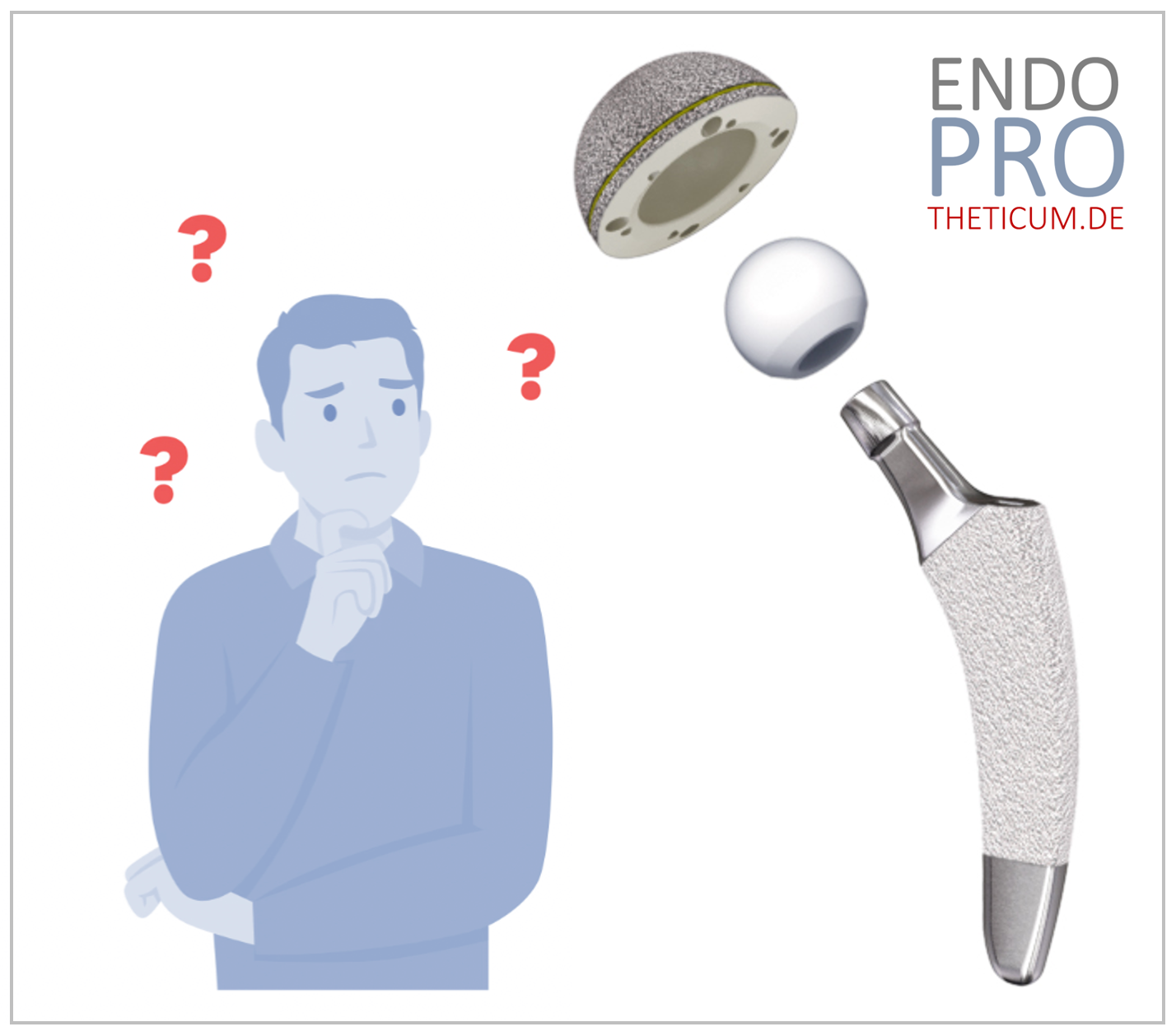
The surgical procedure for implanting a THA takes place in several steps:
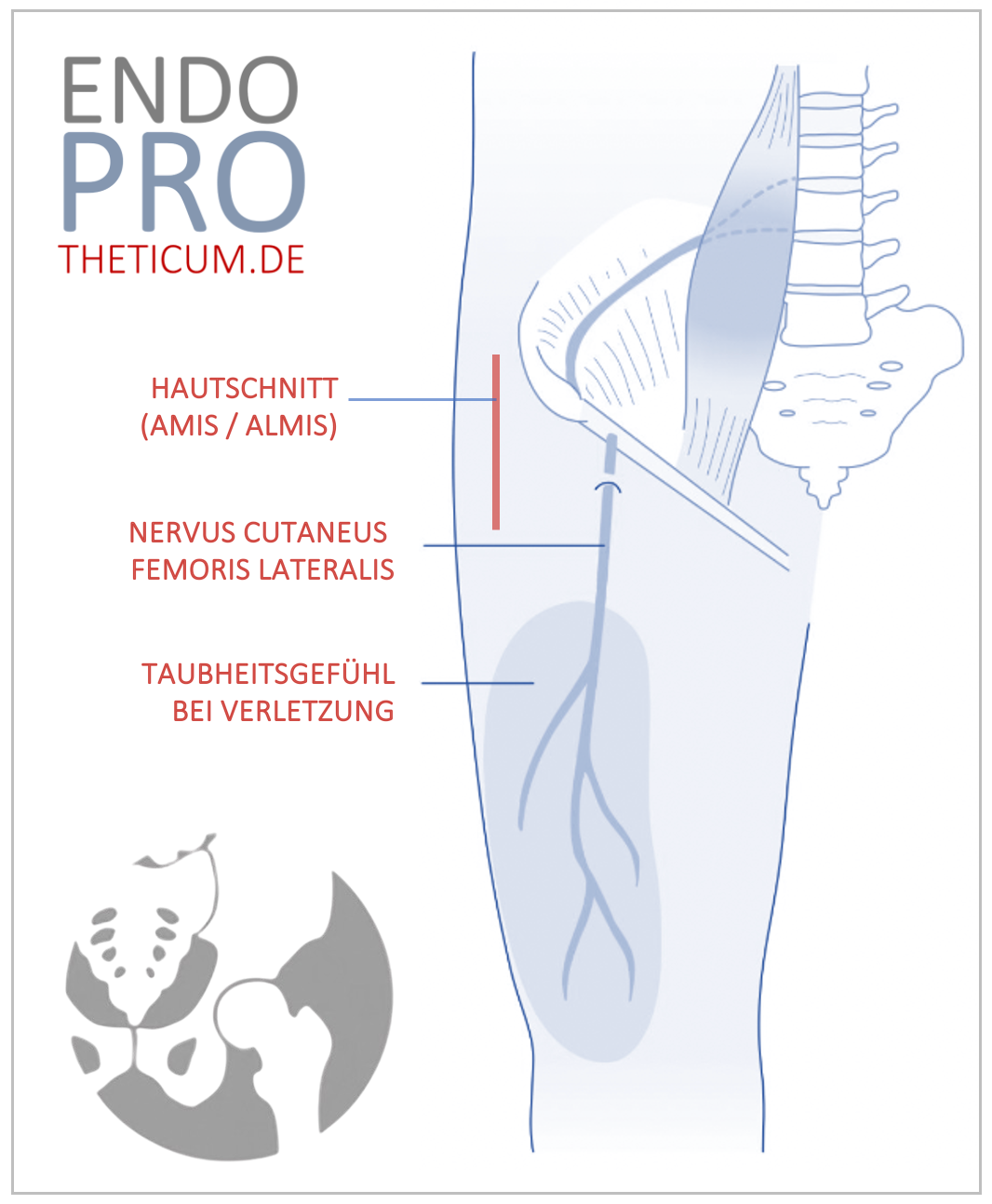
- Access to the hip joint: The hip joint is exposed through a surgical incision.
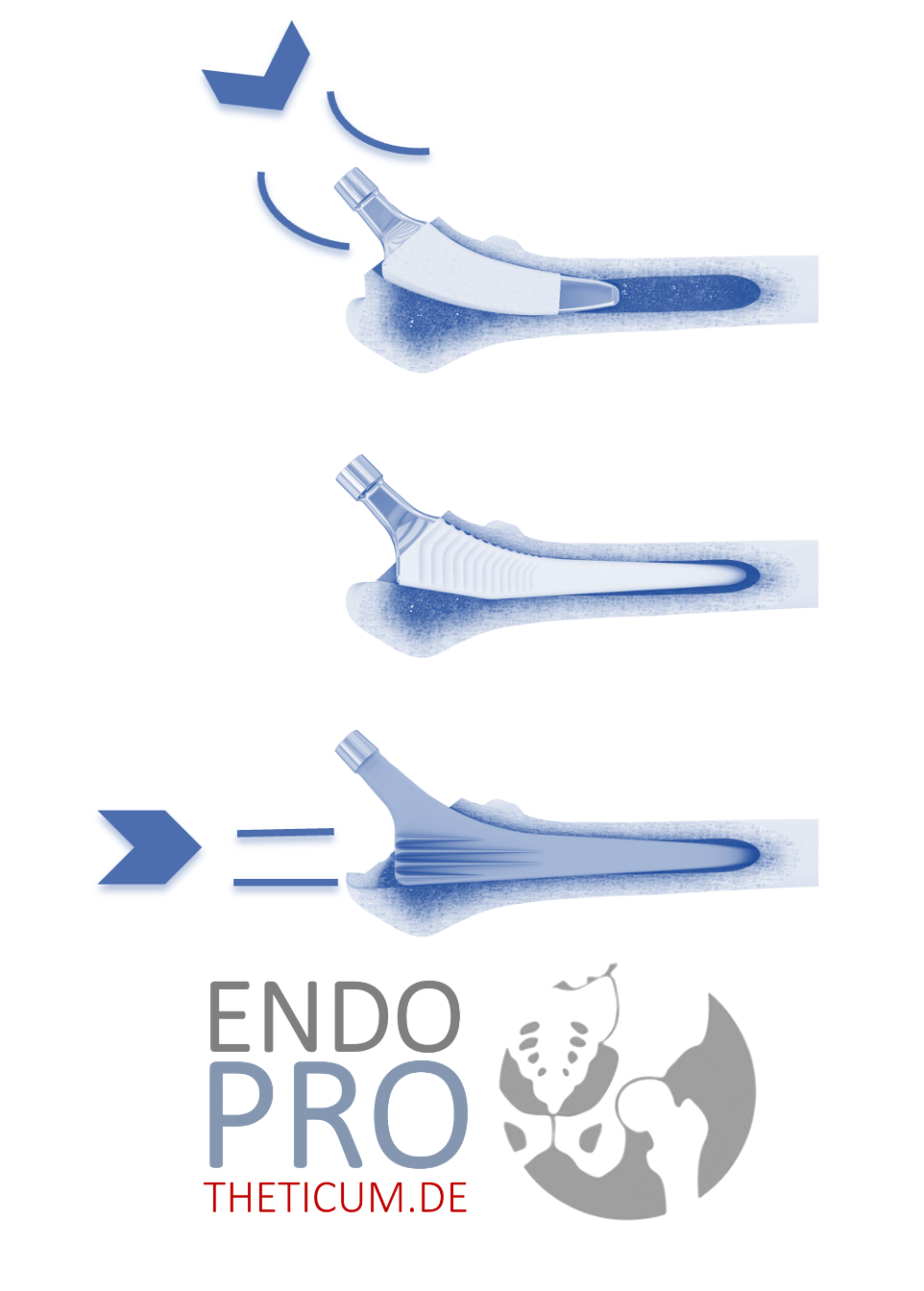
- Removal of the damaged tissue: The damaged femoral head and parts of the acetabular rim are removed.
- Preparation of the bone: The bone is prepared to receive the prosthesis.
- Implantation of the prosthesis: The artificial hip socket and the femoral head are implanted and fixed.
- Wound closure: The surgical incision is closed and healing can begin.
Postoperative rehabilitation after THA for femoral head necrosis
Postoperative rehabilitation is crucial for the success of total hip replacement. The measures include:
- Early mobilization: On the first day after the operation, the patient is encouraged to get up and make his first attempts at walking.
- Physiotherapy: Regular physiotherapy exercises to strengthen muscles and improve mobility.
- Pain management: Adapted pain medication to relieve postoperative pain.
- Follow-up examinations: Regular checks to monitor the healing process and identify possible complications at an early stage.
Prospects of success and long-term results after necrosis of the femoral head
The chances of success of a THA for femoral head necrosis are generally very good. Most patients report a significant reduction in pain and a significant improvement in quality of life. Long-term results show that modern hip replacements can have a lifespan of 15 to 20 years or longer, depending on factors such as activity level and general health.
Risks and complications
As with any surgical procedure, there are risks and possible complications with total hip replacement:
- Infections: Postoperative infections can affect healing and may require further intervention.
- Thrombosis: Blood clots can form after surgery, so prophylactic treatment is important.
- Prosthesis loosening: In rare cases, the prosthesis may become loose and require revision.
- Dislocation: The artificial hip joint can pop out of the socket, which may require another operation.
Conclusion
Femoral head necrosis is a serious disease that, if left untreated, can lead to serious impairments. A total hip arthroplasty (THA) offers an effective solution to relieve pain and restore mobility. Careful preparation, professional execution of the surgical procedure and consistent postoperative rehabilitation can significantly improve the chances of success. Those affected should obtain comprehensive information about the options and choose the best treatment strategy together with Prof. Kutzner at ENDOPROTHETICUM.
MAKE AN APPOINTMENT?
You are welcome to make an appointment either by phone or online .