How sled prostheses can help patients with Ahlbäck's disease
Sled prostheses for Ahlbäck's disease

Ahlbäck's disease, also known as avascular necrosis of the medial femoral condyle, is a degenerative condition of the knee joint that often leads to significant pain and limited mobility. An innovative and effective treatment method for this condition is the implantation of a sled prosthesis, also known as a unicompartmental knee prosthesis. In this blog post, we will dive into the details of this treatment method, examine its benefits and risks, and explore how it can improve the lives of patients with Ahlbäck's disease.
What is Ahlbäck's disease?
Ahlbäck's disease is a form of osteonecrosis that affects the knee joint. It occurs when the blood flow to the bone is interrupted, leading to the death of the bone. This condition can lead to pain, swelling, and limited mobility in the affected knee. The exact cause is unknown, but risk factors include trauma, steroid use, and certain blood clotting disorders.
What is a sled prosthesis?
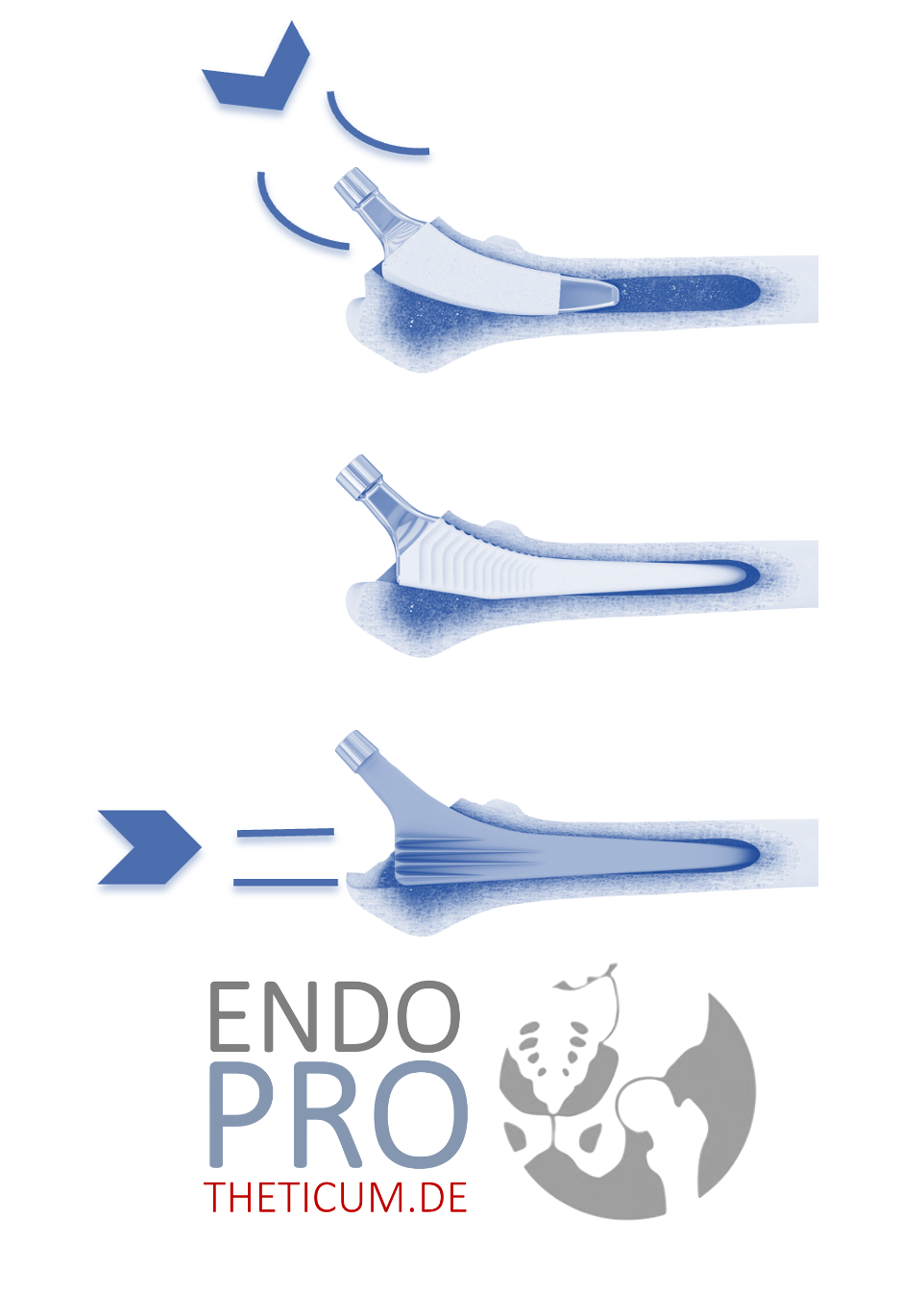
A sled prosthesis is a partial prosthesis of the knee that replaces only one of the two main condyles of the femur (thigh bone). In contrast to the total knee replacement, in which the entire knee joint is replaced, the sled prosthesis allows the preservation of healthy parts of the joint. This method is particularly suitable for patients with localized knee damage, as is common in Ahlbäck's disease.
Advantages of the sled prosthesis in Ahlbäck's disease
- Preservation of healthy bone tissue: Since only the affected condyle is replaced, the healthy part of the knee joint remains intact. This leads to natural joint movement and better functionality.
- Faster recovery: Patients typically recover faster from surgery to implant a sled prosthesis than from a total knee replacement. This means shorter hospital stays and a faster return to normal activities.
- Less postoperative pain: Since the intervention is less invasive and less bone and tissue are affected, patients often report less pain after surgery.
- Improved mobility: The sled prosthesis often allows for greater mobility of the knee compared to total knee replacement.
- Fewer complications: Since the intervention is less extensive, complications such as infections or thrombosis occur less frequently.
The surgical process
- Preparation and planning: Before surgery, a thorough examination is performed, including X-rays and possibly an MRI, to determine the extent of the damage and plan the operation precisely.
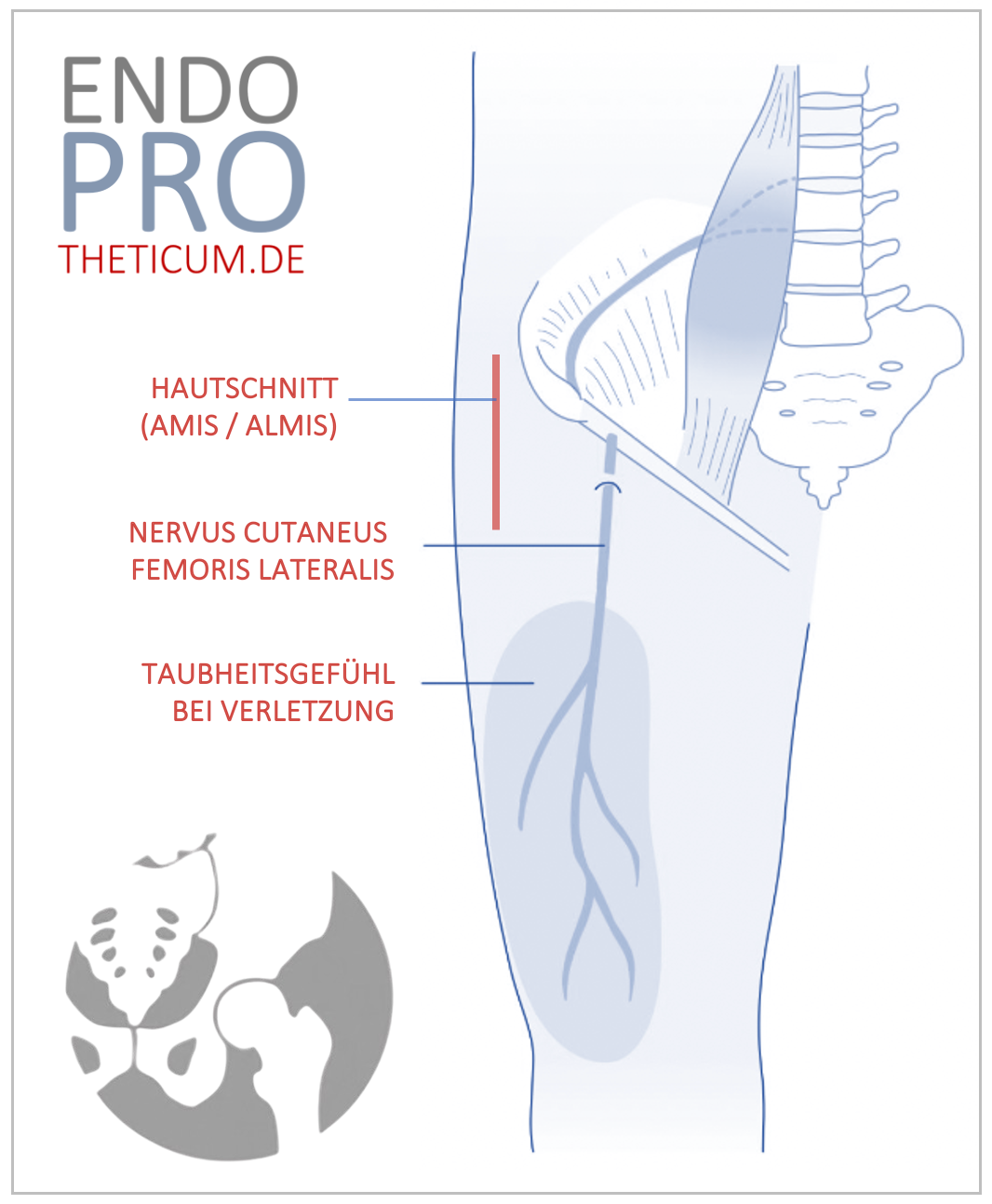
- Surgical intervention: The procedure is performed under general anesthesia or spinal anesthesia. The surgeon makes a small incision over the affected condyle and removes the damaged bone and cartilage tissue. The sled prosthesis is then cemented or fixed without cement in place.
- After the operation: Patients typically spend one to two days in the hospital. Physiotherapy often begins on the first day after surgery to promote mobility and strengthen the muscles.
Aftercare and Rehabilitation
Aftercare and rehabilitation are crucial for the success of the sled prosthesis. An individual rehabilitation plan is created, which includes exercises to strengthen the muscles and improve mobility. Regular follow-up examinations are necessary to monitor the healing process and ensure that no complications occur.
Long-term results
Long-term studies show that patients with a unicompartmental knee replacement often remain pain-free for many years and enjoy a high quality of life. Many patients report a significant improvement in their mobility and a return to activities they were unable to perform before surgery. However, it is essential to note that, as with any surgery, the results can vary individually.
Risks and complications
Although the sled prosthesis offers many advantages, there are also potential risks and complications that need to be considered:
- Infections: As with any surgery, there is a risk of infection. Strict hygiene measures and postoperative care can minimize this risk.
- Thrombosis: After surgery, there is an increased risk of blood clots. Blood thinners and regular exercise help reduce this risk.
- Prosthesis loosening: In rare cases, the prosthesis can loosen, requiring revision.
- Pain and swelling: Postoperative pain and swelling are common, but usually temporary and can be well managed with pain medication and physiotherapy.
Conclusion
The sled prosthesis represents an effective treatment option for patients with Ahlbäck's disease. By preserving healthy parts of the knee joint, it offers numerous advantages over total knee replacement, including faster recovery, less postoperative pain, and better mobility. Nevertheless, it is crucial to consider the potential risks and complications and work closely with the treating physician to achieve the best possible treatment outcome.
Make an Appointment?
You can easily make an appointment both by phoneand online .