Ceramic surface replacement – but is it minimally invasive?
Ceramic hip resurfacing – at the expense of minimal invasiveness

hip replacement surgery today , they quickly realize that medicine is undergoing a small revolution. Just a few decades ago, hip replacement was associated with extensive surgery, a long hospital stay, and frequent complications. Today, hip replacement is considered one of the most successful operations ever performed. Modern implants last for decades, and thanks to minimally invasive techniques , patients are often mobile again just a few days after surgery.
While these minimally invasive techniques have become the standard, an old concept is experiencing a surprising comeback: hip resurfacing . This procedure – often also a cap prosthesis – aims to preserve as much bone as possible. For a long time, however, this idea was burdened by serious complications, particularly metal abrasion .
Now, surface replacement is being discussed in a new form: no longer as a metal-on-metal prosthesis , but as a ceramic cap prosthesis . Ceramics have proven to be particularly wear-resistant and biocompatible in endoprosthetics. Could this be the solution to the problems of the past?
The crucial question, however, is: Can a ceramic surface replacement be implanted using minimally invasive techniques? For patients today, it is taken for granted that hip surgery should be performed through small, muscle-sparing incisions. This reveals a tension: The principle of surface replacement requires a completely different surgical technique, one that is hardly compatible with minimally invasive procedures.
In this article we will explain:
- What exactly is a hip surface replacement?
- Why was the technology in disrepute for so long?
- What does the new ceramic version promise?
- What role do minimally invasive approaches play in modern hip surgery?
- Why are short stem prostheses the safe, bone-conserving and truly minimally invasive solution today?
Finally, you will learn why ceramic surface replacement sounds exciting but has significant disadvantages in practice – and where you can get a modern, minimally invasive hip prosthesis Mainz / Rhine-Main
2. What does hip resurfacing mean?
To understand why surface replacement is such a controversial topic, one must first understand the principle.
2.1 Definition: What is a cap prosthesis?
In a traditional hip replacement, the entire femoral head is removed. A prosthetic stem is inserted into the femur, which is connected to a new femoral head ball. This ball then glides in an artificial socket that is implanted into the pelvis.
Surface replacement works differently:
- The natural femoral head is largely preserved.
- Only the top layer of the bone is removed.
- metallic or ceramic cap is then placed over the femoral head and cemented or anchored.
- This cap, together with a corresponding hip socket, forms the new joint surface.
In principle, it is therefore a kind of "light" hip replacement – the bone is largely preserved, and the anatomy of the thigh is hardly changed.
2.2 Goal: Maximum bone preservation
The most important advantage of surface replacement lies in
bone preservation . This is particularly attractive for younger patients (under 55 years of age) who have a high life expectancy and may eventually require revision surgery.
The more bone that remains in the femur, the easier a subsequent prosthesis implantation will be.
2.3 Differentiation from the classic hip prosthesis
- Standard hip prosthesis (straight stem): complete femoral head removed, long prosthetic stem anchored in the thigh.
- Short stem prosthesis: femoral head removed, but only a short stem anchored in the proximal femur → bone-saving, minimally invasive procedure possible.
- Surface replacement (cap prosthesis): The femoral head is preserved, only a cap is attached.
This places surface replacement between conservative joint preservation (e.g. osteotomy) and classic prosthesis.
2.4 Historical appeal
The idea of replacing a hip joint in a way that preserves the bone has fascinated orthopedic surgeons since the 1970s. It met the wishes of many patients
- change as little as possible about your own body
- at the same time become pain-free and mobile again,
- and keep all options open in the event of a revision.
However, as we will see in the following chapters, the reality of surface replacement had its downsides for a long time.
3. History of surface replacement – from hope to disillusionment
3.1 First attempts in the 1970s
The idea of not completely removing the femoral head , but only covering it with a prosthetic cap, originated in the 1970s. Early models of this so-called hip surface replacement were tested at that time using various materials.
The concept was equally attractive to patients and surgeons:
- Maximum bone preservation – especially valuable for young patients who will have to live with the prosthesis for many decades.
- More natural anatomy – by preserving the femoral neck, the original leverage and muscle attachments are largely maintained.
- Easier revision – if the prosthesis ever needs to be replaced, all options are open, as the bone in the thigh remains largely intact.
However, even the first generations struggled with significant problems: anchoring the caps was technically difficult, and the materials available at the time (e.g., Teflon or early metals) proved to be not very durable. Many implants loosened again after just a few years.
3.2 The Renaissance in the 1990s and 2000s
After a rather disappointing start, surface replacement a comeback in the 1990s. This was mainly due to advances in metallurgy and prosthetic technology .
British orthopedic surgeons Derek McMinn and Ronald F. Treacy developed the well-known Birmingham Hip Resurfacing (BHR) system. It was hailed as a "game changer." Worldwide interest in the hip resurfacing prosthesis rapidly – including in Germany.
Advantages that were highlighted:
- Young, active patients should be able to remain physically resilient for longer.
- The natural movement pattern should be better preserved.
- Bone conservation should facilitate revisions.
Many clinics changed their programs and offered surface replacement as a "modern alternative" to the classic hip prosthesis.
3.3 Metal-on-metal: The great hope
What was special about this generation of femoral head caps was the material : They used metal-on-metal bearing surfaces . This meant that both the cap on the femoral head and the socket in the pelvis were made of highly polished metal.
The hope was:
- Metal is durable and resistant.
- Abrasion should be minimal.
- Larger head sizes should reduce the risk of dislocation (luxation).
Initially, the results seemed promising. Thousands of patients worldwide received such metal prostheses in the early 2000s.
3.4 The problems quickly became apparent – metal abrasion
But complications soon began to mount. After just a few years, the following problems emerged:
- Metal abrasion:
With each step, the cap rubs against the pan. This creates tiny metal particles (cobalt, chromium, nickel) that can enter the body. - Metallosis:
These metal particles accumulate in the surrounding tissue. This leads to inflammation, necrosis (tissue death), and pain. - Systemic metal ion exposure:
Blood tests showed that patients with metal-on-metal caps had elevated cobalt and chromium levels in their blood. This can potentially damage organs – from the kidneys to the heart. - Premature loosening:
Due to tissue damage, many prostheses loosened after only a few years. The originally planned lifespan of 15–20 years was far from being achieved.
3.5 Well-known scandals – the example of ASR
ASR system became particularly notorious . This metal-on-metal system had to be recalled worldwide in 2010 after thousands of patients suffered serious complications.
The consequences:
- Numerous revision surgeries were necessary.
- Worldwide, there were class action lawsuits and billions of dollars in compensation payments.
- Confidence in surface replacement has been severely shaken.
Other systems, such as the BHR prosthesis, also lost acceptance. National registries, for example in Great Britain and Australia, published alarming revision rates.
3.6 Withdrawal from routine
Following these experiences, many clinics decided to no longer routinely offer surface replacement. Professional societies such as the German Society for Orthopedics and Trauma (DGOU) and international institutions also warned against metal-on-metal systems.
Today the following applies:
- Metal-on-metal surface replacement is now only used in exceptional cases.
- Most orthopedic centers have completely abandoned this practice.
- Patients who still have a metal cap prosthesis in their body are regularly monitored (including blood tests for metal ions).
3.7 Lessons from the Past
The history of surface replacement shows how large the discrepancy between theory and practice can be.
Theoretically:
- Bone preservation, natural anatomy, great mobility.
Practical:
- Metal abrasion, inflammation, loosening, systemic risks.
The most important lesson: An implant must not only be technically fascinating – it must also be safe in the long term.
This is precisely where the current discussion begins: If the problem was the material, could surface replacement with a new material – ceramics – be a real alternative?
3.8 Conclusion on the historical section
Hip resurfacing has a turbulent history:
- 1970s: first, largely unsuccessful attempts.
- 1990s/2000s: Boom due to metal-on-metal systems.
- From 2010 onwards: massive problems due to metal abrasion, recalls, loss of trust.
- Today: only a rare indication, but an exciting discussion about new materials.
Patients should be aware that the enthusiasm for surface replacement has always been based on the idea of bone preservation – a goal that remains highly relevant today. However, experience with metal-on-metal restorations has shown how dangerous the wrong choice of material can be.
4. The innovation: Ceramic surface replacement – the comeback of the cap prosthesis?
4.1 Why ceramics?
Following the problems with metal-on-metal prostheses, research focused for a long time on safe, biocompatible materials . Ceramics have already proven themselves in endoprosthetics, particularly in hip sockets and conventional hip prostheses, as being extremely wear-resistant and biocompatible .
The advantages of ceramics at a glance:
- Biocompatibility: Ceramic does not react with the body, no systemic burden from metal ions.
- Low abrasion: Significantly less particle formation in the joint. The risk of metallosis is eliminated.
- Hardness: Ceramic is extremely hard and wear-resistant, which theoretically makes a long lifespan possible.
- Smooth sliding surfaces: Reduce the risk of joint noises or micro-movements that could lead to loosening.
For patients, this means that the cap prosthesis can theoretically from bone preservation without the risks of metal abrasion.
4.2 Structure and Function of the Ceramic Cap Prosthesis
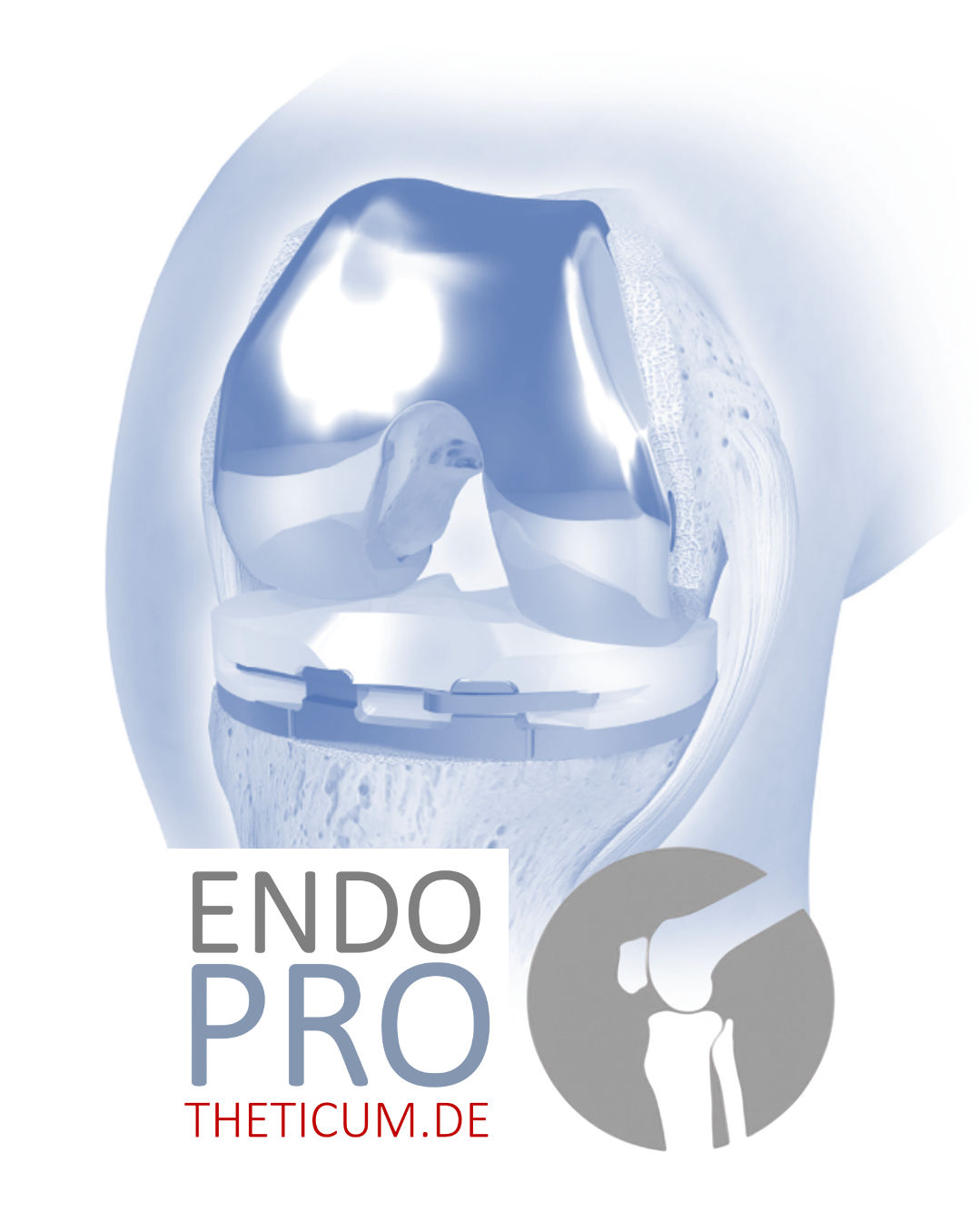
The ceramic cap prosthesis consists of several components:
Ceramic cap for the femoral head:
- It envelops the preserved bone.
- It is cemented or press-fit fixed.
Joint socket:
- Classic TEP pan made of ceramic or ceramic/polyethylene combination.
- It picks up the cap and allows movement.
Fixation mechanism:
- Securing by bone compression or cement.
- Goal: immediate stability, no loosening.
In principle, the ceramic cap replaces the articular cartilage while preserving the natural bone . The joint's range of motion can remain very close to the original anatomy, and the stress on the femoral neck remains physiological.
4.3 Potential benefits for patients
- Bone-sparing:
Preserving the femoral neck is a significant advantage, especially for younger patients or those with higher activity levels. Should revision surgery become necessary at some point, more options are available. - No metal ions:
Unlike metal-on-metal systems, the body is not exposed to metal ions – a crucial increase in safety. - Low abrasion:
Ceramics produce less wear on sliding surfaces, which could reduce the loosening rate in the long term. - Large head size possible:
As with metal cap prostheses, the femoral head can be chosen to be large → lower dislocation rate.
4.4 Challenges and Risks
Despite the theoretical advantages, there are significant limitations :
Ceramic breakage:
While ceramics are hard and wear-resistant, they are also brittle. A break can have catastrophic consequences:
- Sudden instability of the joint
- The need for a complex revision surgery
- Potentially irreversible damage to the femoral head
Technical complexity of the operation:
In order to precisely place the cap on the femoral head, the joint must be dislocated. This means:
- Larger surgical approaches
- More soft tissue damage
- Longer rehabilitation time compared to minimally invasive short-stem systems
Lack of long-term results:
While metal cap prostheses have data over 10–15 years, for
ceramic cap prostheses only pilot studies or small cohorts so far.
- Long-term stability is still unclear
- Large-scale revisions are not sufficiently documented
Limited availability:
Ceramic cap prostheses are currently only offered in specialized centers and not as a standard part of routine operations.
4.5 Current clinical trials and research
In recent years, several research teams worldwide have pilot projects :
- Objective: To check load-bearing capacity, abrasion, risk of dislocation and fracture strength.
- Initial results:
- Low abrasion resistance confirmed
- Dislocation rate low when implanted precisely
- Ceramic fractures are very rare, but possible risk factors have been identified (e.g., mispositioning, suboptimal bone density)
The study authors concluded that ceramics are promising , but have not yet been widely clinically tested. Long-term data (10–15 years) are lacking.
4.6 Patient perspective: Opportunities vs. Risks
For patients, the ceramic cap prosthesis initially sounds like the ideal solution:
- The bone remains intact
- No metal abrasion
- Physiological mobility
But the reality is complex:
- Minimally invasive surgery possible
- The risk of ceramic breakage remains
- Long-term data is lacking → Uncertainty about durability and complications
Patients must weigh the options: Do they prefer an innovative but little-tested technique or a proven, safe alternative such as the short-stem prosthesis , which can be inserted minimally invasively and is demonstrably durable?
4.7 Conclusion Chapter 4
The ceramic cap prosthesis represents the logical next step in surface replacement: bone preservation without the risk of metal.
But:
- Minimally invasive implantation is hardly possible
- Ceramic breakage remains a theoretical but real risk
- Long-term results are lacking
Patients should be aware of these risks and always make the decision in consultation with experienced hip specialists .
5. Minimally invasive hip surgery – the revolution of the last 10 years
Hip surgery has made enormous progress in recent decades. Besides innovations in materials, the focus has been primarily on minimally invasive surgical techniques . For patients, this means shorter hospital stays, less pain, faster mobilization, and less scarring.
5.1 What does “minimally invasive” mean?
The term "minimally invasive" describes surgical procedures that destroy as little tissue as possible while still allowing for safe implantation.
Features of minimally invasive hip surgery:
- Small incisions (approx. 6–10 cm vs. 15–25 cm for classic approaches)
- Muscle-sparing technique: Tendons, muscles and ligaments are not cut, but pushed aside
- Preservation of the joint capsule, if possible
- Goal: faster recovery, less pain, shorter rehabilitation
These techniques are now central to modern hip surgery and have revolutionized patient care.
5.2 The established minimally invasive approaches
Over the last 10 years, the following approaches have become particularly prevalent:
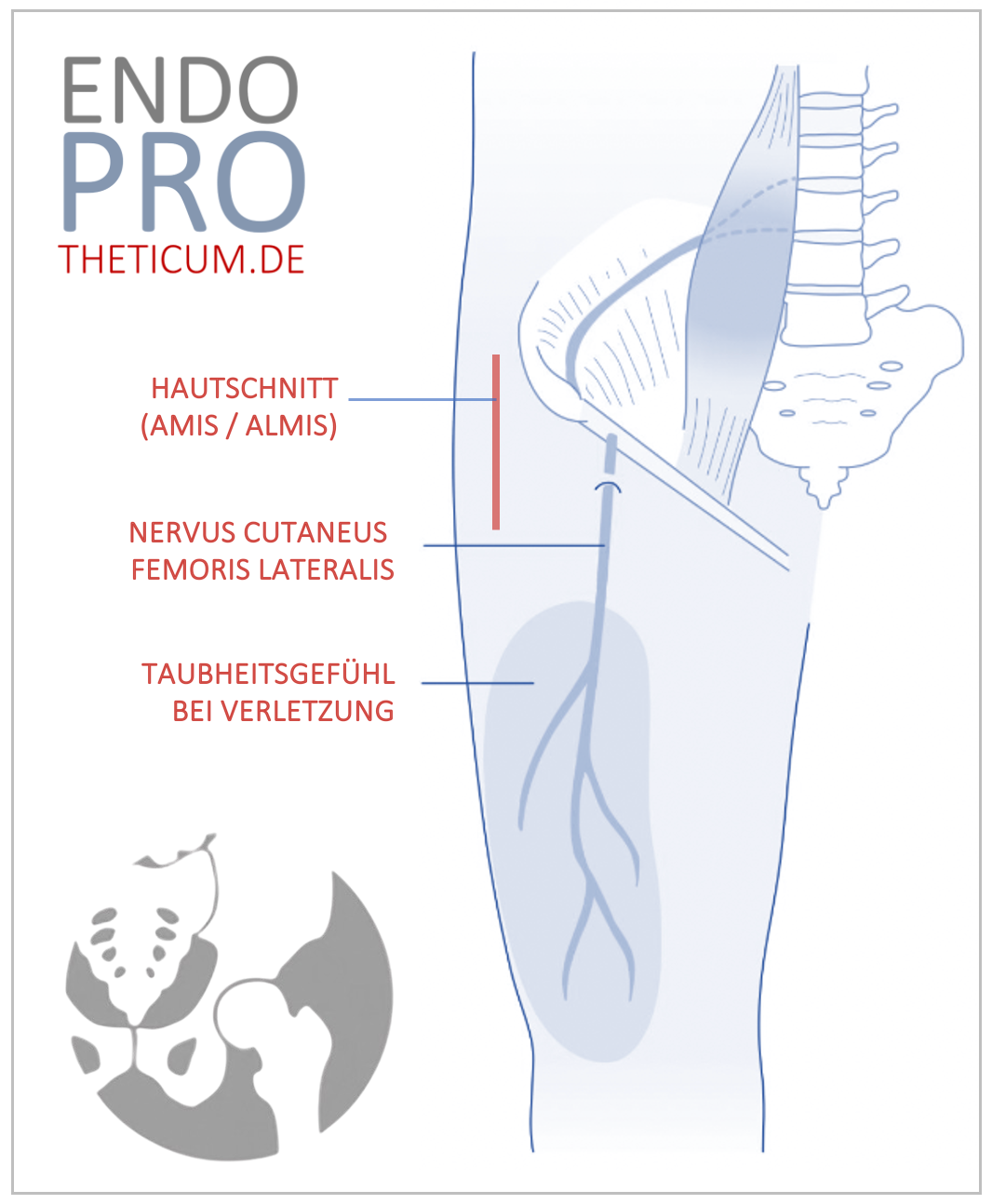
- AMIS (Anterior Minimally Invasive Surgery / Direct Anterior Approach):
- Access from the front, between muscles
- No cutting of important muscle groups
- Very low dislocation rate
- Rapid mobilization possible
- Anterolateral approach (ALMIS):
- Muscle-friendly access, lateral front
- Stable joint guidance, low risk of dislocation
- Proven effective with short-stem and standard prostheses
- Posterolateral approach (PL):
- Access from behind, slightly modified to preserve muscle
- Classical approach, can be adapted minimally invasively
5.3 Advantages for patients
Minimally invasive hip surgeries offer measurable advantages:
Reduced blood loss:
- Gentler muscle preparation → less intraoperative bleeding
- Transfusion rarely necessary
Less postoperative pain:
- Muscles and tendons remain largely intact
- Reduced need for painkillers
Rapid mobilization:
- Patients often get up on the day of the operation or on the first day after the operation
- Shorter hospital stays (2–5 days instead of 7–10)
Cosmetically advantageous:
- Small cuts → smaller scars
- More aesthetically pleasing, especially for younger patients
Improved functional outcomes:
- Muscle strength is restored faster
- Daily life and sports can be done more quickly
These advantages are clinically proven and make minimally invasive approaches a standard in modern orthopedic centers today.
5.4 Evidence and Study Situation
Numerous studies confirm the advantages of minimally invasive hip replacement surgery:
- Shorter hospital stays (reduction of 2–4 days)
- Lower pain score in the first weeks after surgery
- Faster return to normal activities
- Equivalent long-term results regarding implant loosening compared to traditional approaches
Conclusion: Minimally invasive procedures have no impact on long-term stability, but significantly improve postoperative quality of life .
5.5 Why surface replacement cannot truly be implanted minimally invasively
Herein lies the crucial difference:
- During surface replacement, the femoral head must be dislocated in order to precisely position the cap.
- This requires greater access and more soft tissue mobilization.
- Muscles and capsule are subjected to greater stress → a minimally invasive approach is not possible.
Patient perspective:
- Despite the use of modern materials (ceramics), patients do not benefit from the minimally invasive advantages: higher pain, longer rehabilitation, larger scars.
- Minimally invasive surgery is a key feature of modern hip surgery , but it is technically difficult in surface replacement.
5.6 Summary of Chapter 5
- Minimally invasive approaches are now standard in modern hip surgery.
- They enable faster recovery, less pain, and better functional outcomes.
- The ceramic cap prosthesis cannot use these access points because dislocation of the femoral head is necessary.
- This is one of the biggest disadvantages of surface replacement compared to modern short-stem prostheses , which can be implanted minimally invasively.
6. Risks of ceramic cap prostheses
At first glance, the ceramic cap prosthesis seems like the ideal solution: bone preservation, biocompatible material, less wear . However, reality shows that even this modern option is associated with significant risks and uncertainties . Patients should be fully aware of these risks in order to make an informed decision.
6.1 Ceramic breakage – a rare but catastrophic risk
Although ceramics are extremely hard and wear-resistant, they have a brittle structure . This means:
- Under high stress, misalignment, or defects in the bone, the cap can suddenly break .
- A fracture leads to immediate instability of the joint .
- Affected patients require a complex revision surgery , often more involved than with classic short-stem prostheses.
Fact: Even if the probability of a fracture is low, the consequences are serious. Even minor cracks can lead to loosening or pain.
6.2 Soft tissue damage due to necessary dislocation
To place the ceramic cap on the femoral head, the joint be dislocated. This means:
- Muscles, tendons and capsule are stretched or mobilized more.
- Minimally invasive access is not possible because sufficient space is needed for the cap.
- Result: more postoperative pain, longer rehabilitation, higher risk of postoperative muscle weakness.
Patients need to understand: The operation itself is more invasive than a modern short-stem implantation, even though the material is actually innovative.
6.3 Lack of long-term results
While metal cap prostheses have 10–15 years of experience and registry data, only pilot studies or small cohorts exist for ceramic cap prostheses :
- Long-term stability over 15–20 years is unclear
- Revisions in the long term are hardly documented
- Data on physically active patients is lacking
This means that the use remains experimental, even if initial results are promising.
6.4 Patient Perspective
For young, active patients, the cap prosthesis sounds ideal:
- The bone remains intact
- No metal abrasion
- Physiological joint mechanics
However, the disadvantages, such as the lack of minimally invasive access , ceramic breakage , and uncertain long-term results, must be clearly communicated. Patients who value rapid mobilization, short rehabilitation, and safe, proven solutions should explore alternative options.
Modern hip surgery offers proven solutions : e.g., the short stem prosthesis , which is bone-sparing and can be used minimally invasively.
6.5 Transition to modern alternatives
The short stem prosthesis combines the advantages of the cap prosthesis (bone preservation, high mobility) with the advantages of minimally invasive technique :
- Implantation via small, muscle-sparing incisions
- Proven long-term results
- Easier revision if needed
7. Short stem prosthesis as a modern alternative
The short-stem prosthesis has established itself in recent years as the preferred solution for many patients who require hip surgery but value bone preservation and minimally invasive techniques . It combines the advantages of surface replacement with the achievements of modern hip surgery – without the risks of ceramic resurfacing prostheses.
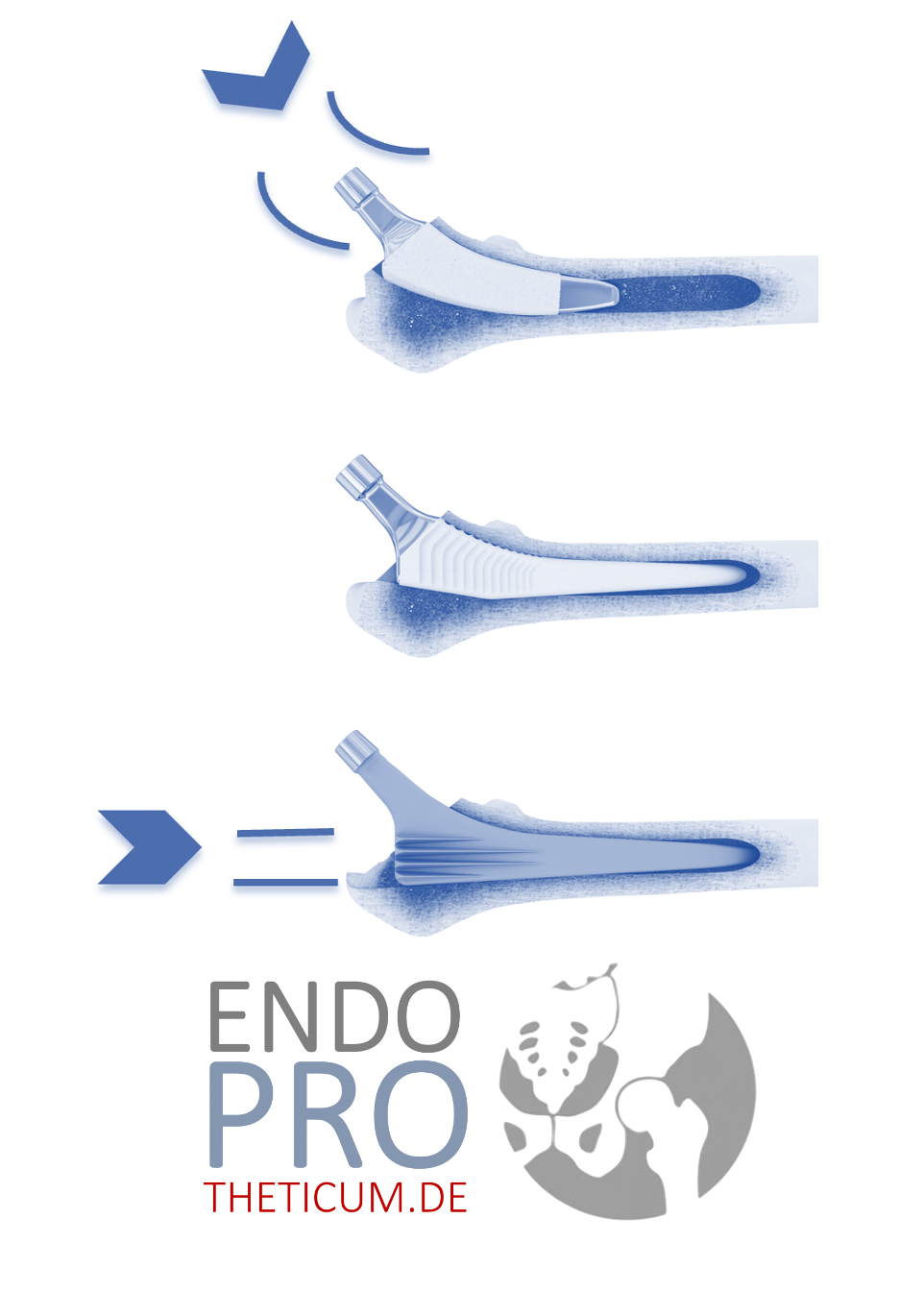
7.1 Structure and Function
The short-stem prosthesis differs from classic hip prostheses in that the stem is shortened and inserted into the proximal part of the thigh:
Short prosthetic socket
- It anchors itself in the upper femur
- Gentler on the bone, less material in the medullary cavity
ball head and socket
- Standardized hip socket made of ceramic or polyethylene
- The ball head can be chosen to be large → low risk of dislocation
Fixation
- Press-fit or cemented, depending on bone quality
- Immediate stability guaranteed
Advantage over cap prosthesis:
- No risky ceramic cap breakage
- Minimally invasive implantation possible
- Long-term results tested
7.2 Minimally invasive implantation
The short stem prosthesis can be implanted via modern approaches :
- AMIS (Direct Anterior Approach): Muscles are spared; patients often stand up on the day of surgery.
- Anterolateral approach: Stable approach, low dislocation rate
- Posterolateral approach: Modified, muscle-sparing, proven
These techniques offer patients the following benefits:
- Less pain
- Faster mobilization
- Shorter hospital stay
- Minor scars
Thus, the short stem prosthesis combines the advantages of the cap prosthesis (bone preservation) with those of minimally invasive hip surgery – a potential advantage over ceramic cap prostheses.
7.3 Evidence and long-term results
Registry data and clinical studies prove:
- Durability: Short stem prostheses have a long lifespan; revisions are easily possible.
- Stability: Low loosening rate, no increased dislocation rates
- Function: Muscle strength and mobility comparable to or better than with classic hip prostheses.
- Patient satisfaction: High, especially among active patients
Conclusion: The short stem prosthesis is not experimental, but proven and safe .
7.6 Short stem prosthesis vs. surface replacement
Brief comparison:
- Surface replacement (ceramic): High bone preservation, minimally invasive implantation impossible, risk of ceramic fracture, experimental
- Short stem prosthesis: good bone preservation, minimally invasive implantation possible, proven technique, easier revision
Conclusion: practical, safe and evidence-based alternative to surface replacement for most patients
For patients in the Mainz and Rhine-Main area, the ENDOPROTHETICUM under Prof. Dr. Karl Philipp Kutzner modern hip surgery with short-stem prostheses:
- Specializing in minimally invasive techniques
- Individual consultation and surgical planning
- High level of professional expertise, modern surgical techniques, excellent aftercare
7.8 Conclusion Chapter 7
- The short stem prosthesis combines bone preservation and minimally invasive implantation.
- Long-term results have been proven, and revisions are simpler than with cap prostheses.
- Patients benefit from faster mobilization, minimal soft tissue damage, and high safety.
- For many young and active patients, it is the best choice when a hip replacement becomes necessary.
8. Surface replacement vs. short stem prosthesis – a direct comparison
The decision between surface replacement (especially ceramic resurfacing) and short-stem prosthesis is often not easy for patients. Both procedures aim to preserve bone and maintain functional hip movement , but differ considerably in safety, surgical approach, and long-term outcomes .
8.1 Bone preservation
Surface replacement:
- Goal: to preserve as much of the femoral head as possible
- Advantage in future revision surgeries
- Risk: In case of complications or ceramic breakage, less intact bone remains
Short stem prosthesis:
- Bone preservation is moderate to high, as only the proximal part of the femur is treated
- Revisions leave more options available
- Advantage: Combination of safety and bone preservation
Conclusion: Surface replacement is theoretically the maximum, short stem prosthesis is practical and safe.
8.2 Minimally invasive approaches
Surface replacement:
- Necessary dislocation of the femoral head
- More extensive soft tissue damage, potentially longer rehabilitation
- Minimally invasive implantation not possible
Short stem prosthesis:
- Implantation is possible via muscle-sparing approaches (AMIS, ALMIS)
- Less soft tissue damage
- Rapid mobilization
Conclusion: Minimally invasive advantages are only achievable with short-stem prostheses.
8.3 Materials and Safety
Ceramic surface replacement:
- Advantages: no metal abrasion, biocompatible
- Risk: Ceramic breakage with catastrophic consequences
- Long-term data are lacking
Short stem prosthesis (ceramic or polyethylene):
- Proven materials, low abrasion rate
- No brittleness, low risk of breakage or loosening
- Long-term data confirm safety
Conclusion: Short-stem prostheses offer proven safety, surface replacement remains experimental.
8.4 Functional Results
Surface replacement:
- Mobility close to the natural hip
- Risk of pain or impaired function in case of complications
Short stem prosthesis:
- Mobility is very good, comparable to surface replacement
- Muscles and tendons remain intact → faster return to everyday life and sports
Conclusion: Functionally equivalent or better with short stem prostheses thanks to minimally invasive techniques.
Patient conclusion:
The short-stem prosthesis combines
safety, bone preservation, and minimally invasive access . Surface replacement sounds attractive in theory, but is riskier in practice and hardly feasible using minimally invasive techniques.
- Ceramic surface replacement is an exciting but experimental process .
- Minimally invasive advantages are not feasible, ceramic breakage remains a residual risk, and long-term results are lacking.
- Short stem prostheses offer proven safety, minimally invasive implantation and bone preservation .
- For patients rapid mobility, short rehabilitation, and long-term security , the short stem prosthesis is the more practical choice.
9. Summary
Deciding to have a hip replacement is a significant step for patients of all ages. Modern procedures offer bone preservation, rapid mobilization, and reliable long-term results , but not every procedure is equally suitable for every individual. This article has thoroughly examined the differences between ceramic resurfacing and short-stem hip replacements .
9.1 Key points at a glance
Ceramic surface replacement (cap prosthesis):
- Goal: maximum bone preservation and physiological joint movement
- Advantages: no metal abrasion, theoretically great mobility, bone-sparing
- Disadvantages:
- Dislocation of the femoral head is necessary → no truly minimally invasive approach
- Risk of ceramic breakage with serious consequences
- Long-term data is lacking; revisions are costly
- Conclusion: Innovative, but experimental and with significant risks
Short stem prosthesis:
- Goal: Bone preservation combined with minimally invasive implantation
- Advantages:
- Minimally invasive procedure possible via AMIS, anterolateral or posterolateral approach
- Proven materials (ceramics, polyethylene)
- Longer shelf life and reliable long-term results (15–20 years)
- Simpler revisions if needed
- Faster rehabilitation and less postoperative pain
- Conclusion: A proven, safe, and patient-friendly solution
9.2 Why minimally invasive is crucial
The last 10 years have shown that minimally invasive approaches are crucial for the success of hip surgery:
- Less soft tissue damage → less pain
- Faster mobilization → shorter hospital stays
- Improved functional results → Faster access to everyday life and sports
Patients who value rapid recovery, minimal pain, and functional safety particularly benefit from minimally invasive techniques – which are unfortunately not feasible in surface replacement.
9.3 Bone preservation vs. safety
Surface replacement sounds attractive because it maximum bone preservation . But practice shows:
- Risks such as ceramic breakage or lack of long-term experience diminish the advantage
- Minimally invasive implantation is not possible → longer rehabilitation, more pain
The short stem prosthesis, on the other hand, offers a balanced solution :
- Bone preservation is good to high
- Minimally invasive implantation
- Long-term results tested
- Revisions simpler and safer
For most patients, the short stem prosthesis is therefore the more practical and safer choice .
9.4 Decision aid for patients
If you are planning hip surgery, you should consider the following points:
Age and activity level:
- Young, active patients particularly benefit from bone-sparing and minimally invasive methods.
Material selection:
- Ceramics offer advantages, metals pose a risk of abrasion, and ceramic cap prostheses are still experimental.
Surgical approach:
- Minimally invasive techniques reduce pain, scarring, and rehabilitation time.
Long-term results and safety:
- Proven systems (short stem prostheses) have been tested over the long term and are revision-friendly.
Individual consultation:
- Every case is unique – detailed consultation with an experienced hip specialist is crucial.
If you are considering hip surgery or would like to learn more about surface replacement, ceramic cap prostheses or short stem prostheses ENDOPROTHETICUM Rhein-Main under Prof. Dr. Karl Philipp Kutzner offers excellent expertise:
- Modern hip surgery with minimally invasive approaches
- Individual consultation to choose the optimal prosthesis
- Long-term proven short-stem prostheses that combine bone preservation and rapid recovery
- Professional aftercare and rehabilitation
- Ceramic surface replacement is innovative, but experimental and involves significant risks.
- Minimally invasive approaches are not possible for surface replacement prostheses.
- The short stem prosthesis offers the perfect balance of safety, bone preservation and minimally invasive implantation .
- Patients benefit from faster mobilization, reliable long-term results, and revision-friendly technology.
- Individual consultation, such as at ENDOPROTHETICUM Rhein-Main, is the key to the optimal decision.
MAKE AN APPOINTMENT?
You are welcome to make an appointment either by phone or online .