Questions to the doctor before joint replacement
25 things you should know before a joint replacement surgery

The decision to undergo joint replacement surgery on the hip or knee is a major step for many people. Often, months or years of pain, limitations, and failed conservative therapies lie behind those affected. At the same time, many questions arise just before the surgery - some are asked, others remain unspoken, although they are crucial for the further course.
This article helps you to be well-prepared and confident in your conversation with your treating doctor. The following questions are among the most important points you should clarify before a joint replacement surgery to have realistic expectations, understand risks, and actively participate in your treatment.
Why good questions before a joint replacement surgery are so important
An artificial joint is not a standard product "off the shelf", but always part of an individual treatment concept. The better informed you are, the better you can:
- Understand decisions
- Build trust
- Reduce anxiety
- Contribute actively to recovery
Many problems after surgery are not caused by the implant itself, but by misunderstandings, incorrect expectations, or unclear communication. Good questions are therefore not a sign of mistrust, but of responsibility.
Question 1: Is joint replacement really necessary for me?
Before it comes to implants, surgical technique or rehabilitation, the most important question is:
Are there still sensible alternatives or is the time for joint replacement actually come?
A responsible doctor will discuss with you:
- how severe the joint wear is
- whether pain and limitations match the imaging
- which conservative measures have already been exhausted
- whether waiting is realistic or rather disadvantageous
A joint replacement should not be done too early, but also not unnecessarily late.
Question 2: What are the alternatives to joint replacement surgery?
Even if an artificial joint is considered, it's worth clarifying whether other options are still viable, such as joint-preserving procedures, partial joint replacement, or temporary conservative measures. An honest assessment is crucial here, whether alternatives realistically help or just bridge time.
Question 3: Which joint should be replaced – and why exactly this one?
Especially with the knee, it's important to understand whether:
- a complete joint is replaced
- only part of the joint is affected
- multiple sections are worn out
This decision has implications for:
- Mobility
- Resilience
- rehabilitation duration
- Long-term result
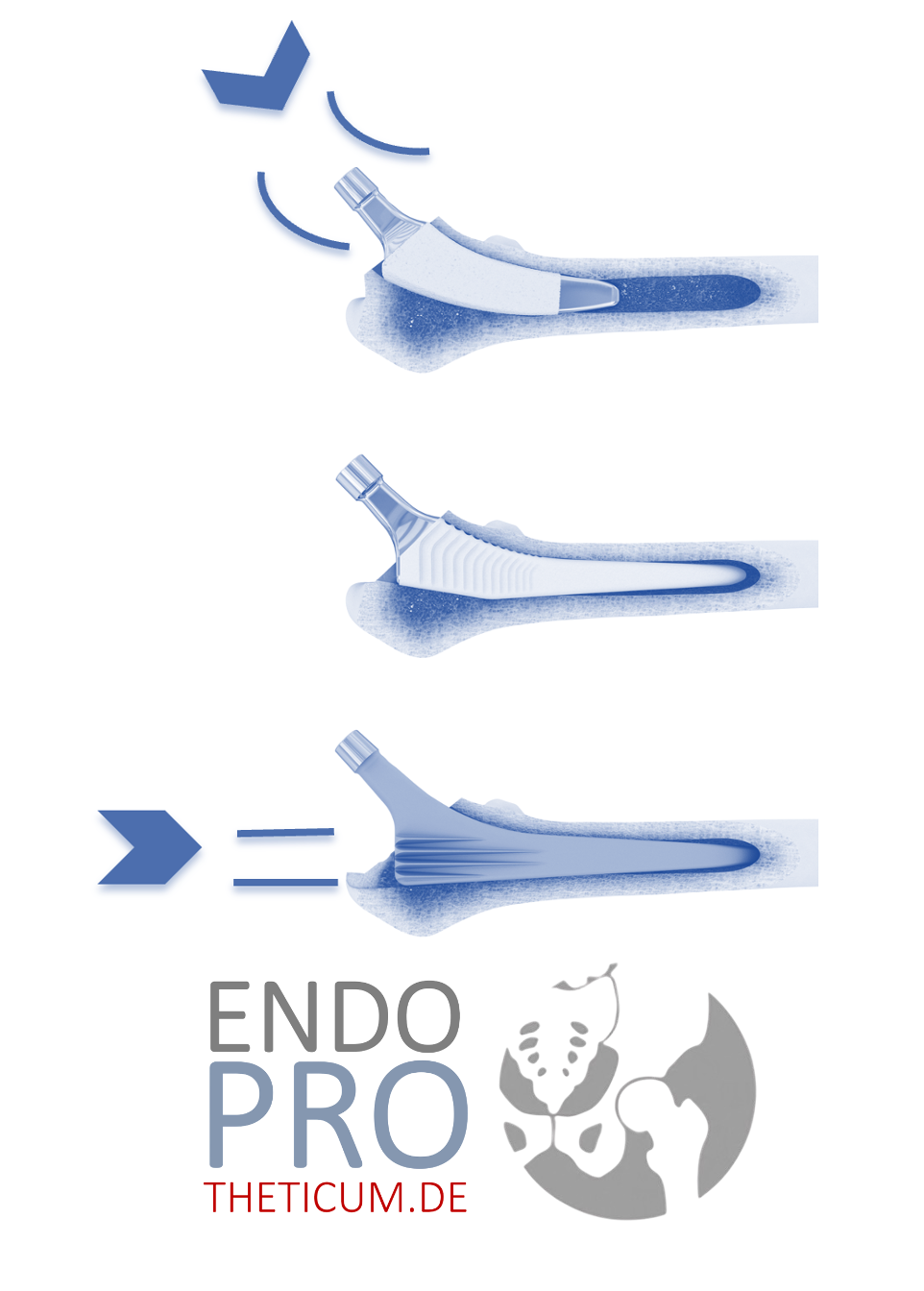
Question 4: What type of prosthesis is intended for me?
Not every prosthesis suits every person. Decisive factors include:
- Age
- Activity level
- Bone quality
- anatomical conditions
Ask specifically why a particular implant is recommended and what its advantages and disadvantages are in your case.
Question 5: How much experience does the surgeon have with this procedure?
This question is legitimate and important. Studies clearly show that routine and specialization have a significant impact on:
- Complication rates
- Surgical duration
- Functional outcome
have. It's not about numbers out of curiosity, but about quality and safety.
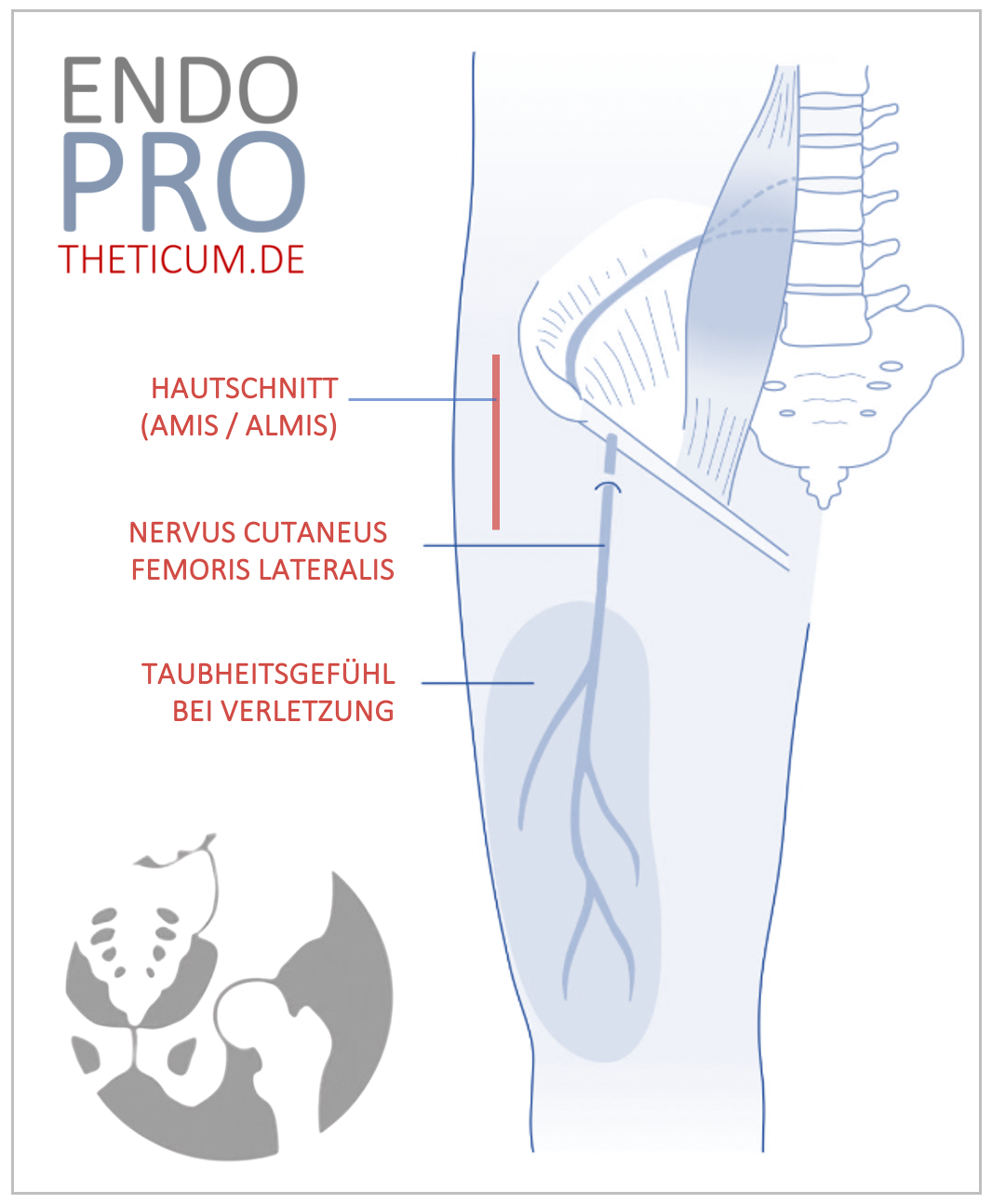
Question 6: How does the operation proceed in concrete terms?
Many fears arise from ignorance. Let it be explained to you:
- how long the surgery lasts
- how the access is made
- what happens during the surgery
- how the new joint is anchored
Who understands what happens feels safer.
Question 7: What risks and complications are there realistically?
Every operation has risks – what matters is how openly and differentiatedly it is discussed. Serious enlightenment means:
- no scaremongering
- no downplaying
- honest assessment of individual risks
Question 8: How severe will the pain be after the surgery?
Pain is one of the biggest concerns for many patients. It is important to know:
- what pain therapy is planned
- how long stronger pain is usual
- when improvement can be expected
Modern pain concepts usually enable a well-controllable postoperative phase.
Question 9: How long will I stay in the hospital?
The length of stay depends on:
- surgical outcome
- mobility
- Comorbidities
- individual healing process
Ask how long a stay typically lasts and what influences earlier or later discharge.
Question 10: When can I get up and walk again?
Early mobilization is now standard. Nevertheless, it is important to know:
- when the first getting up occurs
- whether aids are necessary
- how much load is allowed
👉 This information helps to mentally prepare.
After the operation, the actual path back to mobility begins. Many patients underestimate how important clear post-treatment arrangements are. The following questions help to develop realistic expectations and actively shape your own recovery.
Question 11: What rehabilitation is planned after my operation?
Not every rehabilitation is the same. Clarify whether:
- inpatient rehabilitation
- outpatient rehabilitation
- or intensive physiotherapeutic aftercare
is recommended. Decisive are your personal situation, your environment, and your goals. A well-planned aftercare is at least as important as the operation itself.
Question 12: How long does the overall rehabilitation take?
Many patients hope for a quick return to normality. However, a realistic assessment is important. Ask:
- when everyday movements are possible again safely
- from when longer walking distances are realistic
- when a largely stable resilience is achieved
Rehabilitation does not proceed linearly, but in phases.
Question 13: What role does physiotherapy play – and how long do I need it?
Physiotherapy is not an optional add-on, but a central component of the treatment concept. Clarify:
- how often physiotherapy is recommended
- how long it makes sense
- whether exercises should also be carried out independently
👉 Regularity and correct execution are more important than intensity.
Question 14: Which movements should I avoid at first?
Especially in the first few weeks, there are movements that can put unnecessary strain on the new joint. Ask specifically:
- which degrees of flexion are critical
- whether rotational movements should be restricted
- how to move safely in everyday life
This information provides security and avoids incorrect loading.
Question 15: When can I fully load my new joint?
The permitted load depends on:
- Type of prosthesis
- Anchoring
- Bone quality
- surgical outcome
Have it explained to you in detail, how much load is reasonable when, to avoid overloading or unnecessary relief.
Question 16: How long do I need crutches or aids?
Aids are not a step backward, but part of safe rehabilitation. Ask:
- how long crutches are recommended
- when a gradual waiver makes sense
- which other aids can be helpful
👉 Stopping too early can do more harm than good.
Question 17: When can I drive again?
Driving is an important step towards independence for many. Clarify:
- when reaction time and strength are sufficient
- whether the operated leg is relevant
- which legal aspects need to be considered
Safety always comes before speed.
Question 18: When can I return to work?
Returning to work depends heavily on the type of work. Ask specifically:
- how long you will be unable to work
- whether a gradual return to work is sensible
- which stresses at the workplace may be problematic
👉 Office work is often possible earlier than physically demanding activities.
Question 19: When can I resume sports?
Sports are important – but the right timing is crucial. Have it explained to you:
- which sports are suitable early on
- which are better started later
- which are permanently unfavorable
The goal is long-term joint health, not short-term performance.
Question 20: How long does an artificial joint realistically last?
This question concerns the long-term perspective. The durability depends on:
- load
- Body weight
- Activity level
- prosthesis type
A realistic assessment helps to adjust one's lifestyle sensibly.
Many patients understandably focus strongly on the operation itself. For a good long-term result, however, the weeks, months, and years that follow are at least as important. The following questions help to realistically assess risks and gain security for the time after surgery.
Question 21: How high is my personal risk for complications?
Complications can never be completely ruled out, but their risk varies individually. Ask specifically which factors play a role in your case, such as pre-existing conditions, weight, bone quality, or previous surgeries. An honest assessment helps minimize risks and be prepared.
Question 22: How do I recognize warning signs after the operation?
This is a very important point that is often discussed too little. Let yourself be explained which symptoms are normal and which you should take seriously. These include, for example, persistent severe pain, increasing swelling, redness, fever, or suddenly decreasing resilience. Those who know the warning signs can react early.
Question 23: How high is the risk of infection – and what can I do myself?
Infections are rare but one of the most serious complications. Ask:
- how the risk of infection is minimized
- what hygiene measures are important
- how you can protect yourself before and after surgery
Your own contribution, such as good skin care, dental health, and adherence to recommendations, also plays a role.
Question 24: What does long-term follow-up care look like?
An artificial joint does not require daily attention, but regular check-ups
- how often follow-up examinations are useful
- what examinations are performed
- when you should contact your doctor even without an appointment
Long-term care increases safety and maintains function.
Question 25: What can I do in the long term to ensure my new joint functions well?
This question summarizes many previous topics. Let your doctor explain the role of:
- exercise
- Musculature
- Body weight
- daily behavior
in maintaining the durability and function of your joint. An artificial joint is robust but benefits from conscious handling.
Common misconceptions before joint replacement surgery
Many patients enter the operation with false expectations. These include the assumption that everything will be possible again immediately after the surgery, that pain will completely disappear, or that they will no longer have any influence on the outcome. A realistic understanding protects against disappointment and promotes active recovery.
Summary for patients
A joint replacement operation is not a single event, but a treatment process. Good preparation, open questions, and realistic expectations contribute significantly to success. Those who ask their doctor targeted questions understand decisions better, feel safer, and can actively contribute to their own recovery.
The 25 questions in this article help to ensure that nothing important is forgotten and that you are well-informed before the surgery. They do not replace a personal conversation, but provide a solid foundation for a trusting collaboration between doctor and patient.
Patients who are about to undergo a hip or knee replacement surgery and value comprehensive, understandable, and individualized counseling will find a specialized contact person at ENDOPROTHETICUM Rhein-Main . Under the direction of Prof. Dr. Karl Philipp Kutzner , there is the opportunity to discuss all arising questions regarding necessity, surgical procedure, implant selection, risks, follow-up treatment, and long-term expectations at length. The focus is on transparent education, realistic goal definition, and an individually tailored treatment strategy, enabling patients to make an informed decision for or against joint replacement surgery with confidence.
Make an Appointment?
You can easily make an appointment both by phoneand online .