Secondary osteoarthritis – special features of rheumatoid arthritis
Rheumatoid arthritis and osteoarthritis: Why hips and knees are particularly at risk
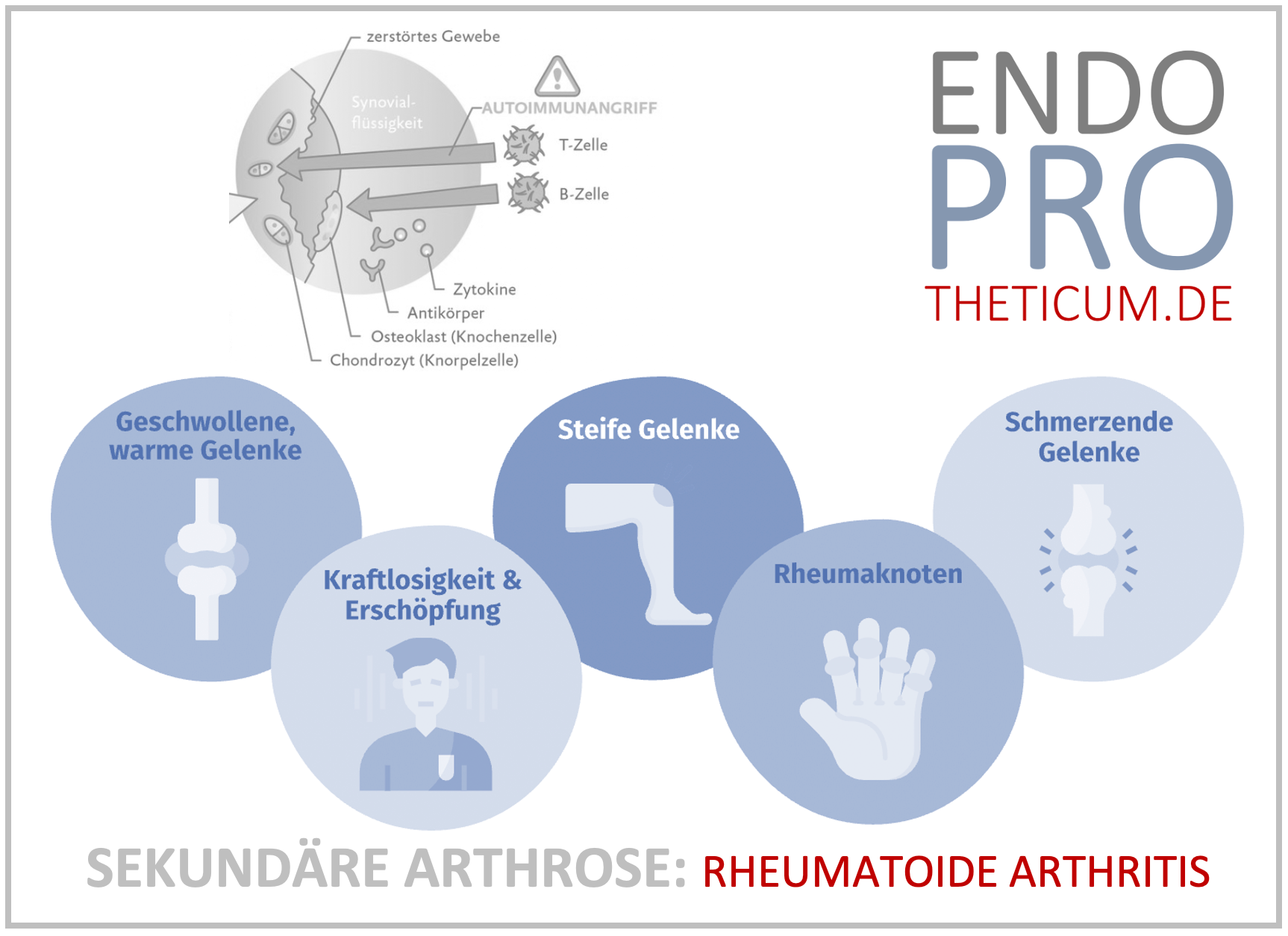
Many people with rheumatism secondary osteoarthritis develops over the years —that is, joint wear and tear triggered by rheumatoid arthritis . Large joints such as the hip and knee are particularly affected. This blog explains in detail how the disease develops, what typical symptoms are, and why, in the final stages, only an endoprosthesis (thigh or knee replacement) is often helpful.
What does secondary osteoarthritis in rheumatism mean?
Osteoarthritis and tear of joint cartilage. In primary osteoarthritis, age and excessive strain are the main factors. In secondary osteoarthritis, however, another underlying disease is involved.
Rheumatoid arthritis is a chronic inflammatory autoimmune disease that leads to the destruction of the synovial membrane, cartilage, and bone. The persistent inflammation leads to severe joint damage over the years. This combination of inflammatory rheumatism and degenerative wear clearly distinguishes secondary osteoarthritis from classic osteoarthritis.
How does osteoarthritis develop due to rheumatoid arthritis?
Inflammation as a trigger
The synovial membrane is permanently inflamed and releases enzymes that break down cartilage tissue.
Bone damage and erosions
In rheumatism, the edges of the bones are literally "eaten away," causing the joint to lose stability.
Misalignments and instability
Damaged ligaments and bones cause O- or X-leg deformities, which place additional strain on the cartilage.
Combination of inflammation and wear
Typically, patients experience both inflammatory pain and osteoarthritis pain – a particularly stressful combination.
Hip joint – secondary osteoarthritis in rheumatism
Symptoms
- Groin pain that can radiate into the leg
- Resting pain and exertion pain
- Limited mobility, especially internal rotation
- Progressive leg length discrepancy
Follow
Hip osteoarthritis in rheumatoid arthritis often progresses more rapidly than in primary osteoarthritis. Those affected lose mobility early and require assistive devices.
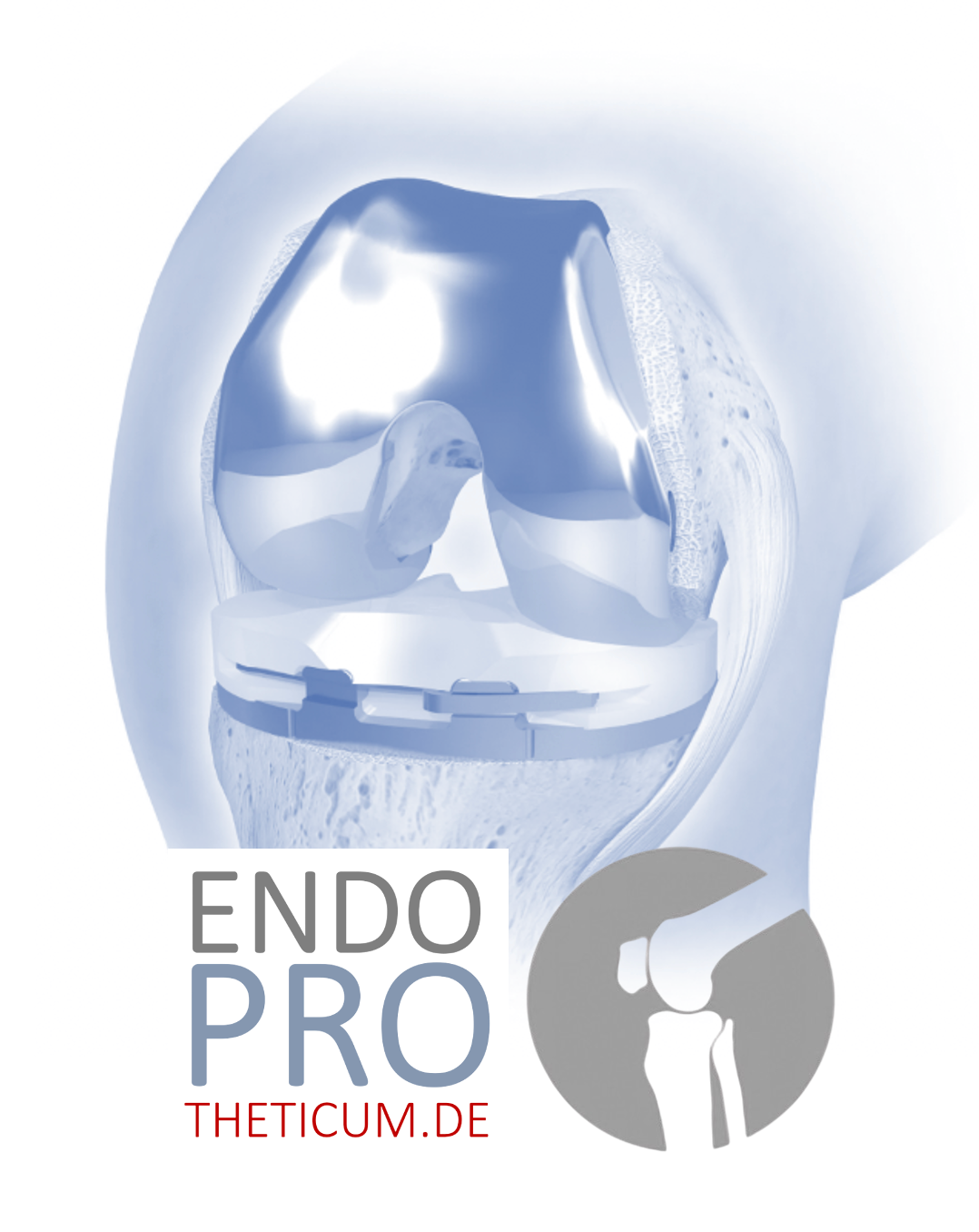
Knee joint – secondary osteoarthritis in rheumatism
Symptoms
- Pain when walking, standing up or climbing stairs
- Recurrent swelling due to synovitis
- Axial deviations (X- or O-legs)
- Significant restrictions in movement
Special feature
In the knee, misalignments are often severe, which makes surgical treatment more difficult.
When is an endoprosthesis (hip replacement, knee replacement) necessary?
When conservative therapies such as physiotherapy, medication, or injections are no longer sufficient, osteoarthritis is referred to as the end stage . Typical signs include:
- Persistent pain, even at rest
- Massive restrictions in everyday life
- Radiologically detectable joint destruction
- Misalignments and instability
In this phase, only an artificial joint (hip or knee replacement) can help.
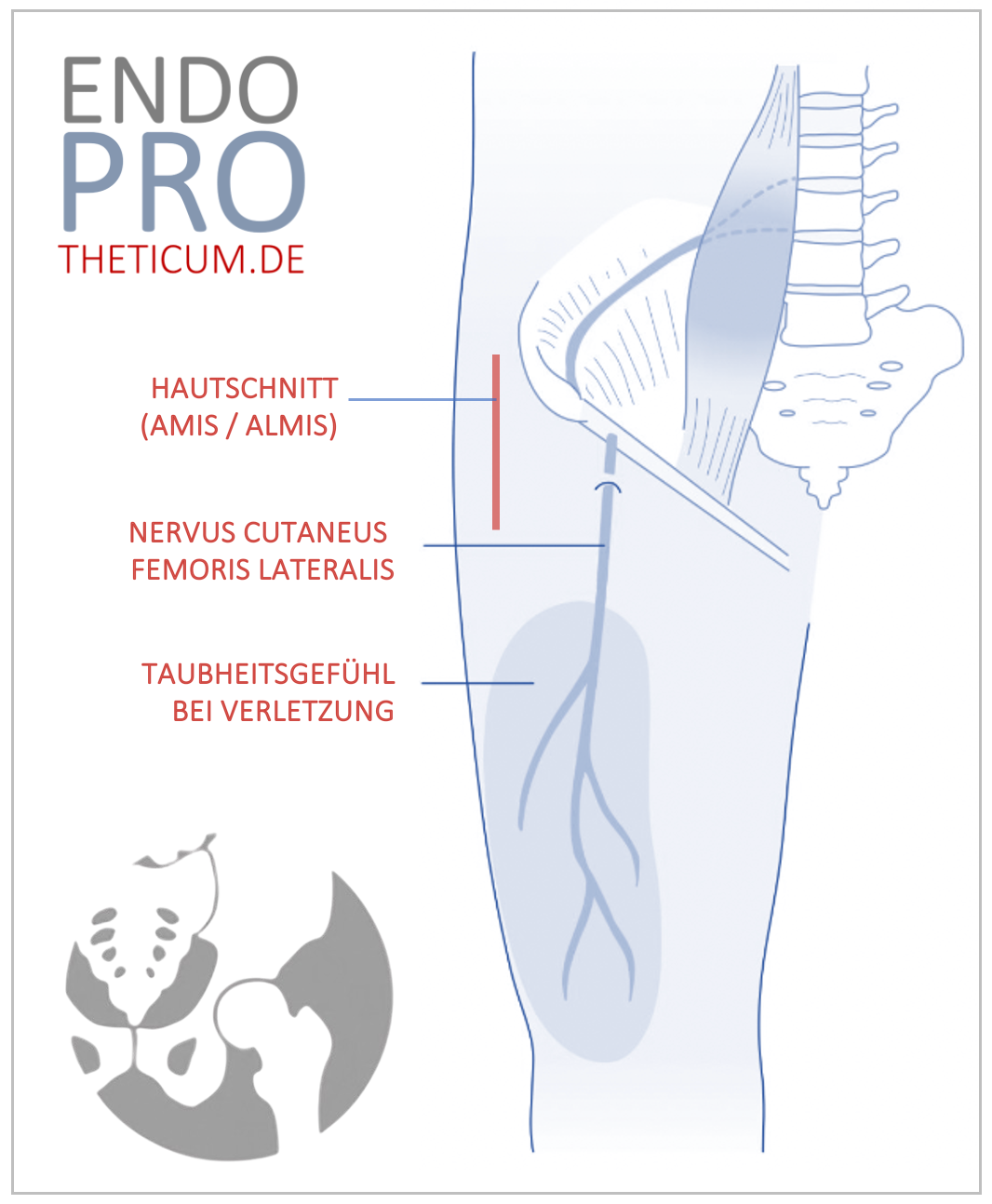
Special features of operations on rheumatic patients
Patients with rheumatoid arthritis differ from osteoarthritis patients without rheumatism:
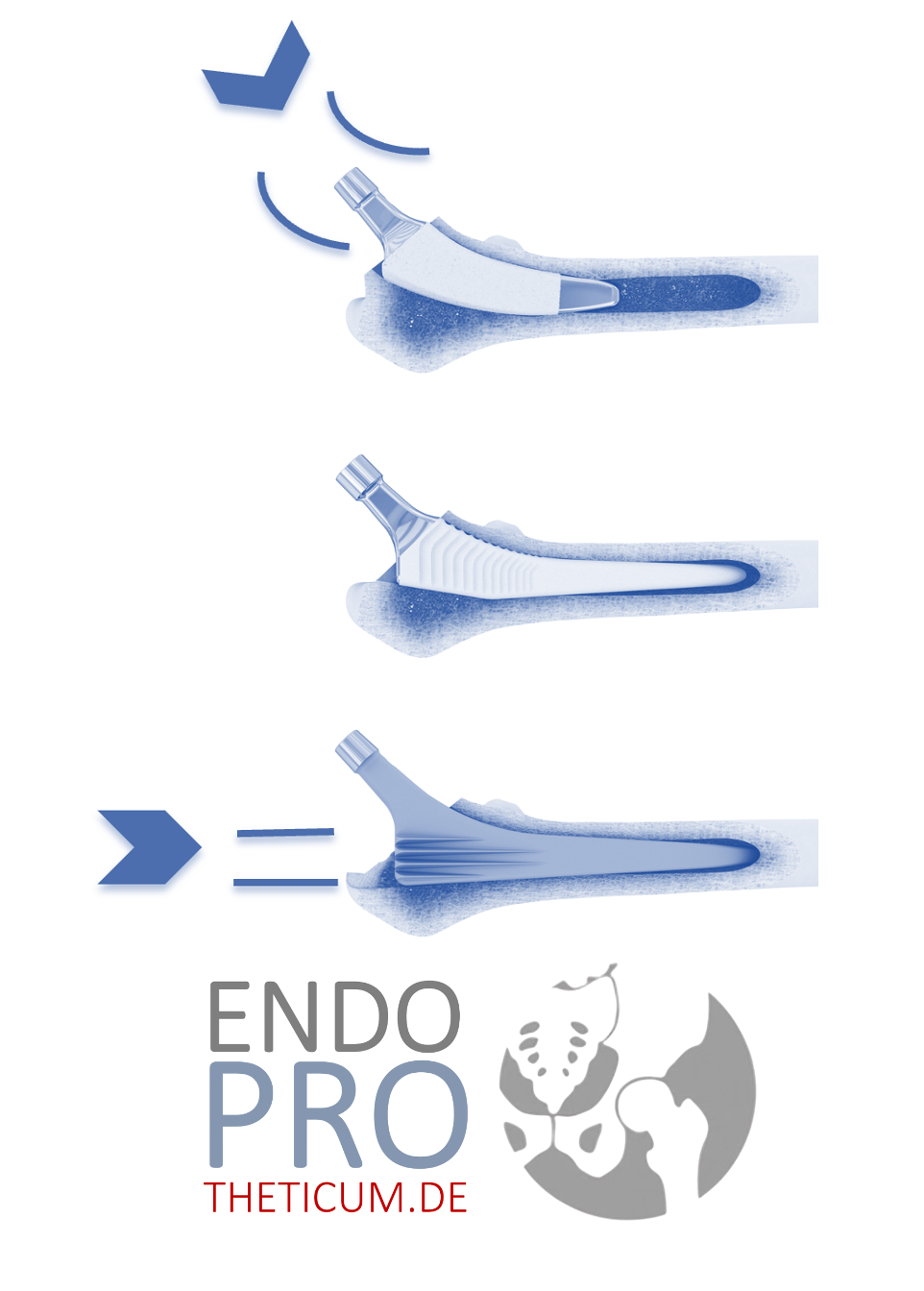
- Bone quality: Often osteoporosis → decision for cemented prostheses
- Soft tissue: Weakened capsule and ligaments require special surgical techniques
- Medication: Immunosuppressants increase the risk of infection → close coordination with rheumatology
- Risk of complications: Wound healing disorders and infections are more common than in primary osteoarthritis
Results after hip and knee replacement for rheumatism
Despite the challenges, studies show:
- Pain decreases significantly after a prosthesis
- Mobility and quality of life improve
- Risks are slightly increased, but can be minimized in specialized centers
Follow-up treatment and rehabilitation
Rehabilitation be individually adapted for rheumatism:
- Early mobilization to prevent muscle loss
- Adapted training due to multi-joint involvement
- Close rheumatological monitoring
- Special wound checks due to increased risk of infection
Why specialized centers are important
Patients with secondary osteoarthritis need experienced surgeons who are familiar with the specific features of rheumatoid arthritis . These include:
- Experience with complex cases
- Availability of special implants
- Interdisciplinary collaboration with rheumatologists
- Individually tailored rehabilitation
Frequently asked questions (FAQ) about secondary osteoarthritis in rheumatoid arthritis
1. What is secondary osteoarthritis?
Secondary osteoarthritis occurs when another underlying disease—such as rheumatoid arthritis —damages the joint cartilage and bones. It differs from primary osteoarthritis, which usually develops due to age and wear and tear.
2. How common is osteoarthritis in rheumatoid arthritis?
Very common. Studies show that almost all patients with long-term rheumatism develop secondary osteoarthritis over time—particularly in the hip and knee .
3. What symptoms indicate secondary osteoarthritis?
Typical are:
- Pain during exercise and at rest
- Joint swelling and stiffness
- Movement restrictions
- Malpositions such as knock knees or bow legs
4. Why are hips and knees particularly affected?
These large joints bear the entire body weight. In cases of rheumatism, they are subjected to additional strain due to inflammation and misalignment.
5. How does osteoarthritis in rheumatism differ from normal osteoarthritis?
Secondary osteoarthritis progresses more rapidly and combines inflammatory pain with wear-and-tear pain , making it particularly stressful.
6. Which therapies help in the early stages?
- Anti-inflammatory drugs (rheumatism therapy, painkillers)
- Physiotherapy and exercise therapy
- Aids such as orthoses or walking aids
- Joint-friendly sports (e.g. swimming, cycling)
7. When is an artificial joint necessary?
If the pain is persistent, mobility is severely restricted, and conservative therapies no longer help, a hip or knee replacement the only option.
8. Are surgeries riskier for rheumatism?
Yes, osteoporosis, weakened soft tissue, and medications slightly increase the risk of infections and impaired wound healing . However, these risks can be minimized in specialized centers.
9. Which prostheses are suitable for rheumatism?
Cemented prostheses are often recommended because bone quality may be reduced. Modern implants can be individually adapted to the joint situation.
10. How long does an artificial joint last for rheumatism?
Even in cases of rheumatoid arthritis , hip and knee prostheses usually last for many years. Modern materials make service lives of 15–20 years or more possible – provided optimal aftercare is provided.
11. How does rehabilitation proceed after a prosthesis for rheumatism?
Rehabilitation to the individual. Important factors include:
- Gentle early mobilization
- Training of several joints, as often not only one joint is affected
- Close monitoring by orthopedics and rheumatology
12. Why should you have surgery in a specialized center?
Because they have experience with complex rheumatic cases. The ENDOPROTHETICUM Rhein-Main, under Prof. Dr. Kutzner, offers, for example:
- Individual prosthesis planning
- Special surgical techniques for rheumatism patients
- Interdisciplinary collaboration with rheumatologists
The ENDOPROTHETICUM Rhein-Main – Expertise in rheumatism and arthrosis
Under the direction of Prof. Dr. Karl Philipp Kutzner, the ENDOPROTHETICUM Rhein-Main specializes in hip and knee arthroplasty – even in complex cases such as secondary osteoarthritis caused by rheumatism.
Special benefits for patients:
- Modern surgical techniques (e.g. short-stem hip prostheses, modular knee implants)
- Tailor-made rehabilitation programs
For patients with rheumatoid arthritis this is the optimal care in the end stages of osteoarthritis.
Conclusion
Secondary osteoarthritis in rheumatism is a complex condition that particularly affects the hip and knee joints. The combination of inflammation and wear and tear quickly leads to the final stage. Conservative therapies can slow the process but cannot stop it. In the final stages, hip or knee arthroplasty offers the only permanent solution.
Thanks to modern implants, precise surgical planning, and specialized centers such as the ENDOPROTHETICUM Rhein-Main under Prof. Kutzner, patients with rheumatoid arthritis can now lead a pain-free and active life again, even with secondary osteoarthritis.
MAKE AN APPOINTMENT?
You are welcome to make an appointment either by phone or online .