Hip replacement (hip prosthesis)
Hip replacement in Mainz & Rhine-Main – Endoprosthetics Center

1. Introduction – Significance of hip replacement in modern orthopedics
Total hip replacement (THR) is one of the most successful surgical procedures in orthopedics and trauma surgery today. Hardly any other surgical intervention offers a similar combination of:
- reliable pain reduction
- regained mobility
- improved quality of life
- very high long-term durability of modern implants
In Germany, around 240,000 hip replacements performed annually – and this number is rising. Demographic change, increasing life expectancy, and higher mobility demands in old age mean that more and more people need a total hip replacement – and more and more patients are actively seeking reliable information.
The following guide is therefore deliberately extremely detailed, medically professional, SEO-optimized, and yet written in a way that is easy for patients to understand. It is intended to:
- Approaching people who are about to undergo hip surgery,
- to inform medically interested readers,
- as well as providing search engines with a maximally structured, high-quality and comprehensive resource.
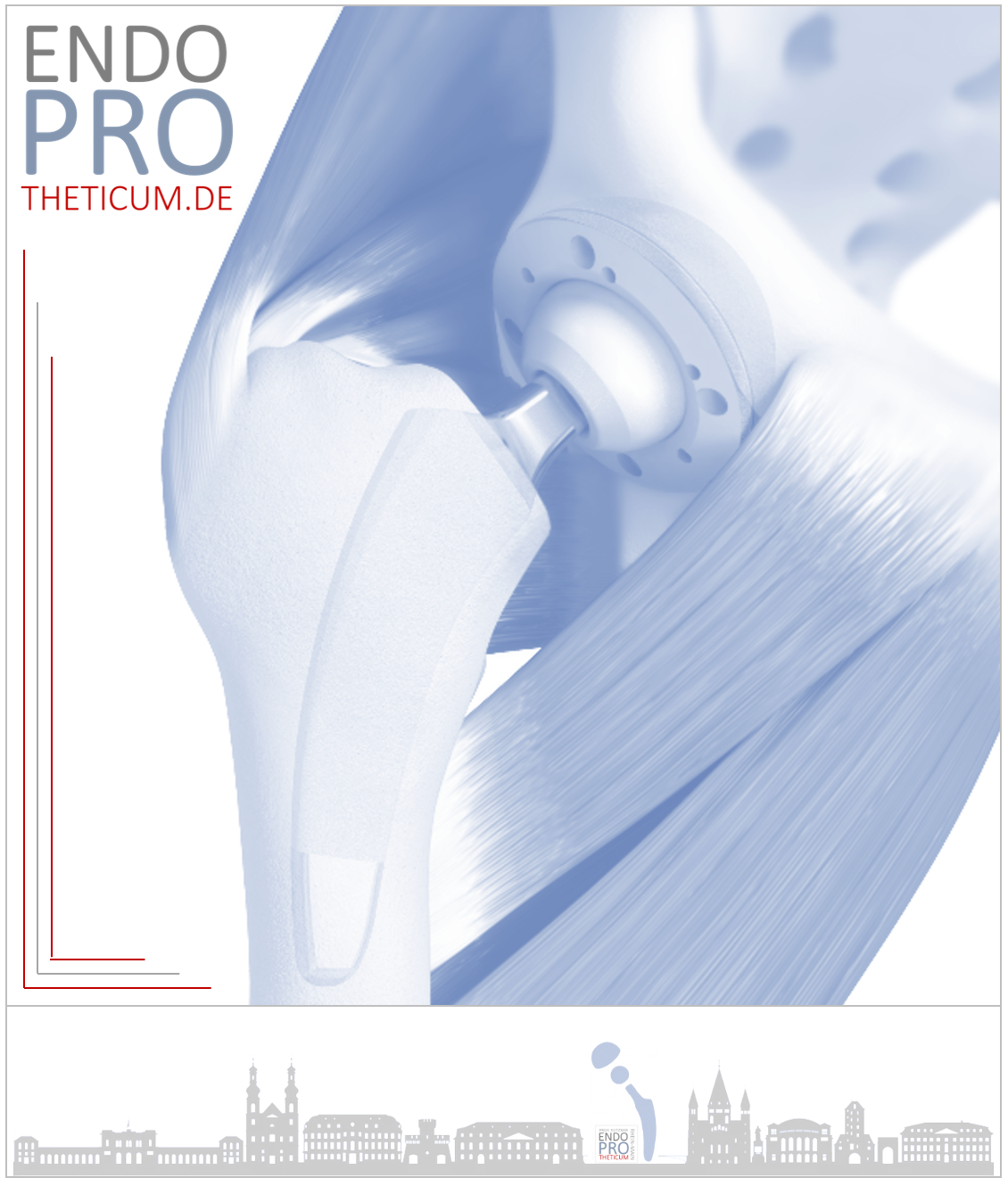
2. Anatomy of the hip joint – Why the joint is so vulnerable
The hip joint is one of the largest and most important joints in the human body. It is a ball-and-socket joint , consisting of:
- Femoral head (head of the femur)
- Acetabulum (hip socket)
- cartilage covering
- articulated lip (labrum)
- joint capsule
- surrounding muscles (especially gluteal muscles)
Why does the hip joint become diseased?
Typical causes include:
- Primary osteoarthritis (most common cause)
- rheumatism
- Circulatory disorders (femoral head necrosis)
- Malpositions (e.g. hip dysplasia)
- Consequences of the accident
Depending on the cause, cartilage abrasion, joint inflammation, instability or structural damage can occur, which cannot be reversed over time.
3. Indications for hip replacement – when is the right time?
The decision to have a hip replacement is an individual one – but medically clearly definable. The decisive criteria include:
3.1. Severe pain despite conservative therapy
The measures that have been exhausted include:
- physical therapy
- NSAIDs (ibuprofen, diclofenac etc.)
- Intra-articular injections
- Physical Medicine
- Weight loss
- Movement therapy
If all of this is no longer sufficient, surgery is a sensible option.
3.2. Reduction in quality of life
Typical warning signs:
- Pain when walking below 1,000 meters
- nighttime pain
- Problems putting on shoes
- Limping / Gait disturbance
- Restrictions on professional or sporting activities
3.3. Progressive joint destruction as seen on X-ray
Radiologically visible signs:
- Joint space narrowing
- subchondral sclerosis
- Osteophytes
- deformed femoral head
- Cyst formation
3.4. Further reasons
- Joint misalignment
- advanced necrosis
- pronounced rheumatic changes
4. Preoperative diagnostics: The path to safe planning of a total hip replacement
Modern hip replacement surgery requires precise and standardized diagnostics:
4.1. X-ray in two planes
Standard diagnostics for determining:
- Joint wear
- Joint geometry
- leg length
- Femur shape (Dorr classification)
4.2. CT or MRI (for specific questions)
e.g. in the case of:
- Dysplasia
- Deformities
- post-traumatic changes
- Revision cases
4.3. Clinical examination
Assessment of:
- Leg length discrepancies
- Rotation capability
- Adduction/abduction deficits
- Pain location
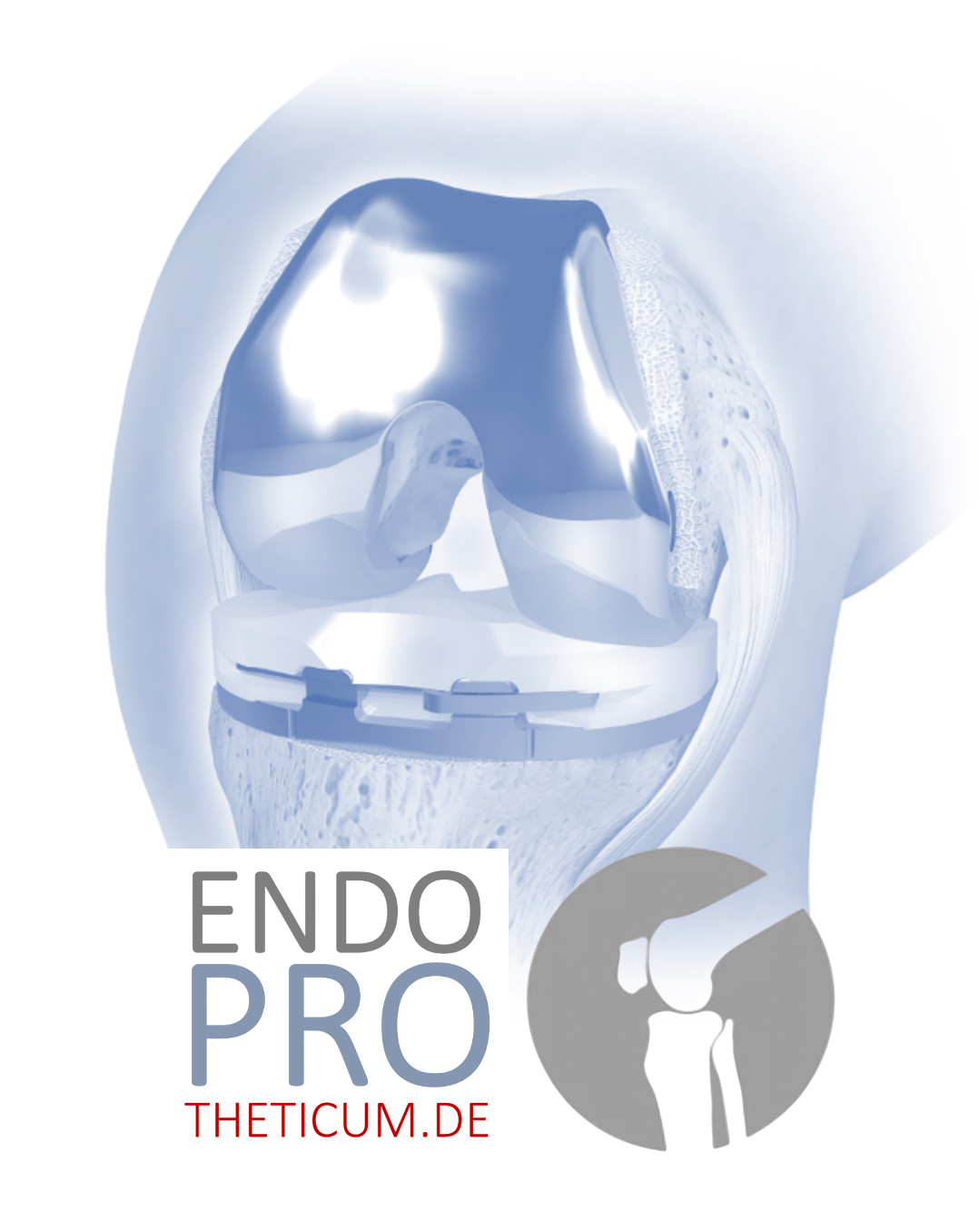
5. Modern Implants – Structure, Materials, Durability
A total hip replacement essentially consists of four components:
- Shafts (for anchoring in the femur)
- Pan component
- Inlay (insert in the pan)
- Head component
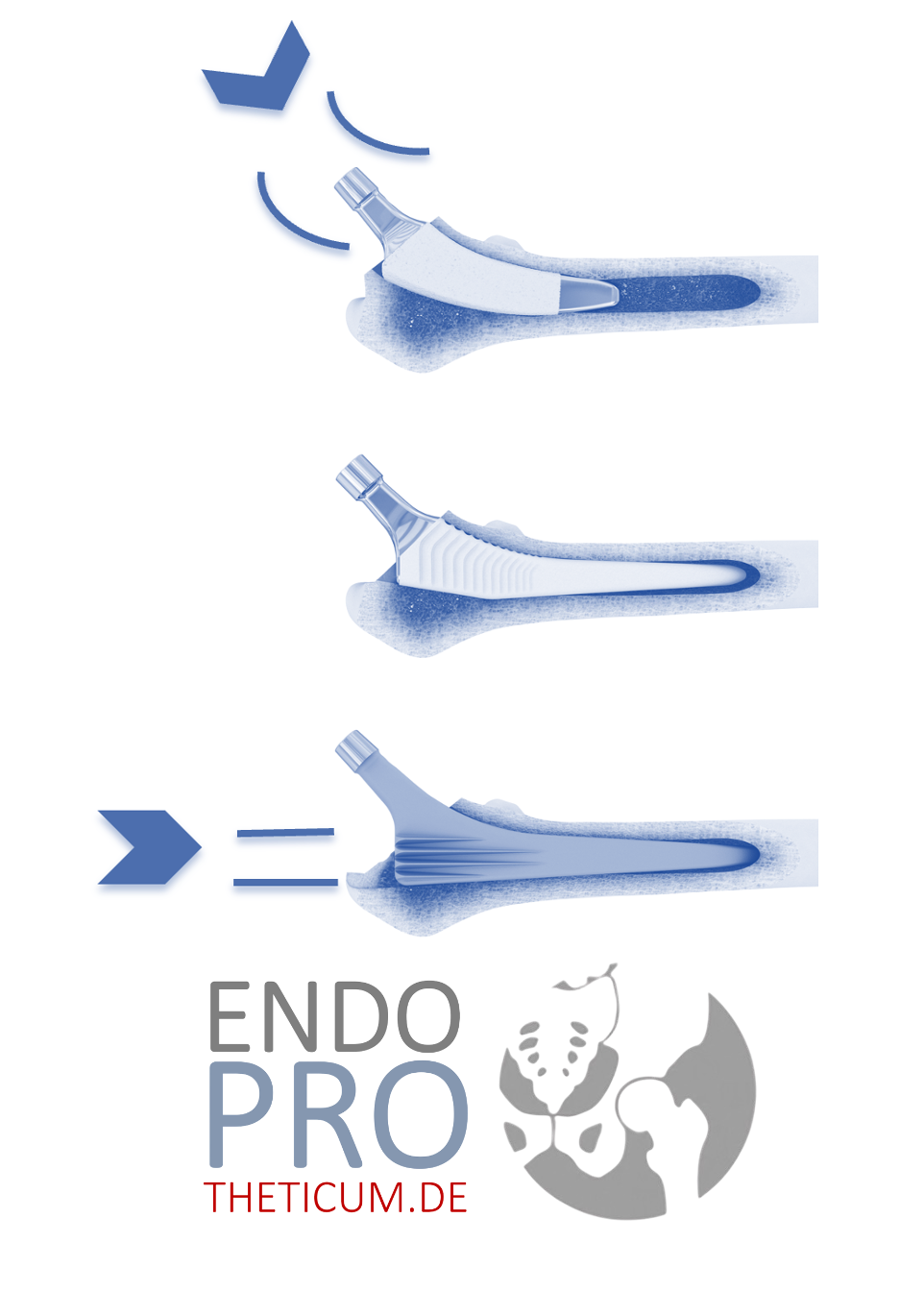
5.1. Shaft designs
- Straight line
- Short shaft
- Femoral fixation (cementless)
- Cemented shafts
Short stem prostheses offer advantages in terms of:
- bone-sparing surgery
- faster rehabilitation
- natural power transmission
- favorable for younger patients
5.2. Pans
Cement-free – standard in Germany.
Cemented – for poor bone quality.
5.3. Materials
- Titanium (stem & cup) – very good biocompatibility
- Ceramic heads – extremely low wear values
- Polyethylene inlays (highly cross-linked PE)
5.4. Abrasion & Service Life
Modern implants now achieve a lifespan of 20–30 years , often longer.
6. Surgical approaches to hip replacement – advantages and disadvantages
The following dominate in Germany:
6.1. Anterior Approach (AMIS / DA)
Advantages:
- gentle on the muscles
- less blood loss
- faster mobilization
6.2. Lateral Approach (Watson-Jones / Hardinge)
Advantages:
- good overview
- very stable
6.3. Posterior approach (Moore / Kocher-Langenbeck)
Advantages:
- easily accessible
- suitable for complex cases
Disadvantage:
- slightly higher risk of dislocation (now very low thanks to modern technology)
7. Operational Procedure – Step by Step
- anesthesia
- Skin incision
- Showing the joint
- Femoral head removal
- Inserting the pan
- Inserting the shaft
- Attaching the head
- Test mobilization
- Wound closure
Duration:
45–90 minutes
Blood loss: significantly less than before (often <300 ml)
8. Risks and complications of hip replacement
Even though hip replacement surgeries are extremely safe, the following risks must be mentioned:
- Infection (approx. 0.5–1%)
- Luxation (0.5–2%)
- Thrombosis / embolism (rare thanks to prophylaxis)
- Leg length difference
- Nerve injury (rare)
- Relaxation in the long term
Professional centers work with standardized protocols to further minimize these risks.
9. Rehabilitation after hip replacement – modern standard
Day 0–1: Early mobilization
- Getting up on the day of surgery or the following day
- Full weight-bearing is possible with modern implants
Weeks 1–3
- Everyday mobility
- Gait training
- Climb stairs
Weeks 4–12
- Muscle building
- normal everyday activities
After 3–6 months
- sporting activities (cycling, Nordic walking, swimming)
10. FAQ – Frequently Asked Patient Questions about Hip Replacement on the Internet
- How long does a hip replacement last?
- Which is better: cemented or cement-free?
- Which sports are allowed after hip replacement surgery?
- How much pain is there after the operation?
- How long will I be unable to work?
- What can I do again immediately – and what can't I?
- Are there any movements I should avoid?
- What to do if you experience cracking or pulling sounds in your artificial hip joint?
- Can a hip replacement also be used in younger people?
- How much does a hip replacement cost?
- How do I find the best hip center?
All questions will be answered in detail in the next section.
Recommendation 11 – Why specialized centers deliver the best results
A clear, independent medical trend of recent years is:
→ The higher the specialization, the lower the complication rate and the better the long-term results.
Specialized facilities such as Endoprotheticum and specialized clinics with a high number of cases (e.g., curaparc-clinic Mainz) offer:
- standardized, highly optimized processes
- state-of-the-art implants
- minimally invasive procedures
- individual planning
- significantly lower risk of complications
- Excellent rehabilitation facilities
Conclusion:
For optimal results, surgery in a specialized center with high expertise in primary and revision endoprosthetics is strongly recommended.
12. Detailed answers to the most frequently asked patient questions
12.1. How long does a modern hip replacement last?
Modern hip implants now achieve impressive longevity. The decisive factors are:
- Material quality
- correct positioning
- Bone situation
- Patient activities
- body weight
- Aftercare
Lifespan of modern implants
Current scientific data show:
- 90–95% of modern hip prostheses function for at least 20 years .
- Many prostheses now last 25-30 years or longer .
- Short-term stocks show similarly good results when correctly indexed.
Influence of age
- Younger patients (<60 years) use the prosthesis more intensively, therefore the wear and tear may be higher.
- Older patients benefit from a long, usually lifelong, implant lifespan.
In short:
With modern materials such as ceramic-ceramic or ceramic-PE, service lives of 20–30 years are now normal – often significantly longer.
12.2. Which is better: cemented or cement-free?
Both systems have clear indications:
Cementless hip prosthesis
The standard at:
- good bone
- younger patients
- normal bone quality
- stable bone structure
Advantages:
- Bone ingrowth
- Long-term, very stable fixation
- simple revision option
cemented hip prosthesis
Ideal for:
- osteoporosis
- very soft bone
- older age
- High-risk patients
Advantages:
- immediate, stable anchoring
- Lower intraoperative fracture rate in cases of poor bone quality
Which one is "better"?
It's not the method that matters – but the right combination of patient and implant .
12.3. Which sports are allowed after a hip replacement?
The following generally applies:
Allowed / recommended:
- Ride a bike
- Hike
- To swim
- Nordic Walking
- Gym (controlled strength training)
- Cross-country skiing
- golf
- moderate jogging (depending on the initial situation)
Allowed with caution:
- Tennis (Doubles)
- light jogging
- E-bike
Not recommended (higher risk):
- football
- squash
- Snowboard
- intense basketball
- Extreme sports
Basic rule:
Movement is good – jerky, rotationally intensive impact loads are worse.
12.4. How painful is a hip replacement?
Modern anesthesia and surgical techniques significantly reduce pain.
Typical course:
- Days 0–2: Wound and muscle pain
- Days 3–7: significantly decreasing
- Weeks 2–4: primarily muscular complaints
- From week 4 onwards: increasingly pain-free
The often-described "freedom from osteoarthritis pain" occurs for many within the first 48 hours .
12.5. How long will I be unable to work?
Depending on profession:
- Office work: 3–6 weeks
- Light physical occupations: 6–10 weeks
- physically demanding jobs: 10–14 weeks
12.6. Which movements should be avoided initially?
That depends on the surgical approach.
Posterior approach:
- strong bending above 90°
- Crossing the legs
- strong inward rotation
Anterior approaches:
- fewer restrictions
- Nevertheless, no extreme positions in the first 6 weeks
12.7. Is it possible to fly with a hip replacement?
Yes, anytime. Important:
- Observe thrombosis prophylaxis
- regular movement during the flight
12.8. Can a hip prosthesis squeak or crack?
Rarely can be caused by:
- Tendon friction
- Scar tissue
- Muscular imbalance
A harmless noise may occur.
Actual denture squeaking is rare and usually due to the material, but hardly relevant with modern implants.
12.9. What to do in case of pulling, stabbing, or pressure sensations?
Mostly muscular.
Typical: iliopsoas muscle, gluteal muscles, tensor fasciae latae.
If symptoms persist → consult a doctor.
12.10. How much does a hip replacement cost?
- Those with statutory health insurance: fully covered by health insurance
- Privately insured patients: dependent on additional costs according to the German Medical Fee Schedule (GOÄ).
- Self-payers: €10,000–€20,000 depending on the facility
12.11. Can a hip replacement be performed at a young age?
Yes – increasingly common.
Modern implants are bone-conserving (short stems) and long-lasting.
13. Detailed presentation of modern implant types
13.1. Short stem prostheses – a modern, bone-saving solution
Short stems primarily act on the proximal femur and protect:
- Market space
- diaphyseal portion
Indication:
- good bone quality
- younger patients:
- anatomically suitable femur shape
Advantages:
- accelerated rehabilitation
- more physiological power transmission
- lower fracture rate in long-term studies
13.2. Standard straight shaft
Still the gold standard, proven in:
- primary endoprosthetics
- complex cases
- older patients
Long-term data show excellent survival rates even after 30 years .
13.3. Ceramic head components
Characteristics:
- extremely low abrasion
- excellent biocompatibility
- good aging stability
Abrasion values <0.01 mm/year → practically immeasurable.
13.4. Polyethylene inlays (Highly cross-linked PE)
The most modern PE is cross-linked by irradiation and shows:
- extremely low abrasion
- high long-term stability
14. Operational Details: In-depth Technical Insight
This section is aimed particularly at readers with a medical interest:
14.1. Pan positioning (Lewinnek safe zone)
Angle:
- Inclination: 40° ± 10°
- Anteversion: 15° ± 10°
Good positioning minimizes:
- Dislocation risk
- abrasion
- Edge load
14.2. Shaft positioning
Goal:
- Neutral position
- Stable anchoring in the femur
- No varus/valgus
14.3. Leg Length Management
An important quality feature.
The following is measured:
- intraoperatively using a template
- clinically via leg axis analysis
- possibly via navigation / robotics
14.4. Navigation & Robot Assistance
Modern assistance systems promise:
- higher precision
- improved reproducibility
- ideal for complex anatomical situations
Some specialized centers are already using this technique.
15. Complication management in hip replacement – modern strategies
15.1. Dislocation
Frequency:
0.5–2%
Management:
- closed reposition
- Movement adjustments
- Possibly switching to dual-mobility systems
15.2. Infection
One of the most feared complications.
Symptoms:
- Redness
- Overheating
- Fever
- nighttime pain
Therapy:
- Debridement
- Flush
- Soft tissue management
- Possibly two- or one-time changeover
Specialized centers offer particularly high success rates.
15.3. Easing
Early easing of restrictions (rare):
- often infectious or mechanically caused
Late easing of restrictions:
- mostly abrasion particle reaction
- Bone resorption
Therapy:
- Revision with long shaft
- Pan replacement
- Possibly pelvic bowls
16. Long-term outcome – How does a hip replacement develop over decades?
16.1. 1–2 years after surgery
- full load capacity
- stable muscles
- normal gait
16.2. 5–10 years after surgery
- still stable
- minimal abrasion
March 16th, 10–20 years
- Minimal abrasion
- Risk of easing restrictions is low
16.4. >20 years
- depending on the implant type
- Low revision rate
17. Extended FAQ
1. Can a hip replacement slip out of place?
Yes, but rarely. Modern surgical techniques minimize the risk.
2. Is it possible to have an MRI scan with a hip replacement?
Yes, modern implants are MRI-compatible.
3. Can I drive again right away?
After approximately 2-4 weeks, depending on the side (right vs. left).
4. Can you feel the prosthesis?
No – it is fully integrated into the body.
5. How quickly will one recover?
Daily life: 3–6 weeks, sports: 8–12 weeks.
6. What does "full load" mean?
Walking without restrictions, depending on the pain threshold.
7. Does a hip prosthesis need to be adjusted?
No – there is no mechanical adjustment.
Recommendation 18 – Why specialized centers are crucial for hip replacement
Patients benefit from:
- high level of experience
- standardized processes
- shorter surgery times
- lower complication rates
- better long-term results
- modern navigation and short shaft technology
Specialized centers (e.g. Endoprotheticum & curaparc-clinic Mainz) now offer the safest and most reproducibly best form of hip replacement care in Germany.
6. Hip surgery: explained step-by-step
Hip replacement surgery is now a highly standardized procedure with excellent long-term results. Modern surgical techniques, optimized implants, and specialized centers have made the procedure safer, less invasive, and more reliable. Nevertheless, it remains a major orthopedic surgery, the quality of which depends significantly on the surgeon and the center .
6.1 Preparing the operating room
The procedure is performed in a highly sterile environment. This includes:
- laminar airflow
- sterile floor coverings
- complete surgical draping of the patient
- Use of the latest navigation and imaging systems (depending on the center)
The difference in quality between many clinics is already evident here.
Specialized endoprosthetics centers , which perform several hundred to a thousand hip replacements annually, generally have more modern operating infrastructure, well-coordinated teams, and standardized procedures.
6.2 Patient Positioning: Side-lying or supine position?
The patient's position depends largely on the chosen surgical technique.
Side position
Frequently used in posterior and lateral approaches.
Advantages:
- good overview
- reliable visualization of the acetabulum
- established technology with long experience
supine position
Typical for minimally invasive approaches (AMIS, DAA).
Advantages:
- ideal setup for intraoperative imaging
- excellent control of leg length
- less soft tissue trauma
6.3 Skin incision & soft tissue access in hip replacement (approaches in detail)
6.3.1 Minimally Invasive Direct Anterior Approach (DAA, AMIS)
The DAA is currently one of the most popular approaches, especially in specialized centers.
It runs intermuscularly and internervously between the tensor fasciae latae and the sartorius muscle.
Advantages:
- Muscle conservation
- rapid mobilization
- low risk of dislocation
- anatomical reconstruction
Disadvantages:
- steep learning curve
- potential lesion of the lateral femoral cutaneous nerve
- Impaired vision in muscular patients
6.3.2 Anterolateral approach (Watson-Jones)
Also gentle on the muscles, as it is predominantly intermuscular.
Advantages:
- good overview
- minor soft tissue damage
- fewer dislocations than posterior
6.3.3 Lateral approach (Hardinge)
Once the standard access point.
Advantages:
- excellent dislocation safety
- robust representation
Disadvantages:
- Detachment of the gluteus medius is possible
- risk of postoperative Trendelenburg symptoms
6.3.4 Posterior approach (Kocher-Langenbeck)
Still one of the most common access points worldwide.
Advantages:
- optimal view of the shaft
- easy to learn
- very flexible
Disadvantages:
- higher risk of dislocation
- Soft tissue transection of the short external rotators
7. Hip replacement surgery – step by step
7.1 Illustration of the hip joint
After opening the joint:
- Dislocation of the femoral head
- Illustration of the acetabulum
- Femoral head ablation
- Exposing the pan
7.2 Acetabular preparation
1. Removal of the labrum and articular cartilage
The acetabulum is completely exposed down to the subchondral bone.
2. Reaming
The milling process is carried out in defined steps. The following is important:
- correct center point
- Maintaining the anatomical inclination (38–45°)
- correct anteversion (15–25°)
3. Inserting the pan component
Depending on the type:
- Pressfit pan
- screw pan
- cemented pan
- double-bowl pan
4. Inlay implantation
Typical materials:
- Polyethylene (XLPE)
- Ceramics
- Metal (now rare)
7.3 Femur preparation
Step 1: Opening the market space
Using special rasps and reamers.
Step 2: Rasting to the final size
Goal:
- optimal primary stability
- anatomical reconstruction of leg length
- correct rotation
Step 3: Inserting the shaft
Types:
- Short shaft
- Standard
- Proximal vs. diaphyseal fixation
- Cemented vs. cement-free
Step 4: Attaching the prosthetic head
Materials:
- Ceramics (AMZ, Delta)
- Metal (CoCr, rare)
8. Intraoperative control: Leg length, offset & stability
8.1 Leg length (LLD – limb length discrepancy)
One of the most common concerns for patients.
Use specialized centers:
- intraoperative imaging
- Navigation systems
- digital leg length measurement
- mechanical reference points
- Navigation pins and offset tools
8.2 Offset Reconstruction
Important for:
- Muscle tension
- Gait
- Dislocation prevention
- Power transmission
8.3 Dislocation Testing
The surgeon checks:
- end-range mobility
- posterior and anterior impingement point
- Stability in flexion, rotation and adduction
9. Wound closure
The closure is achieved through multiple layers:
- Reconstruction of the musculature (if detached)
- Fascial closure
- Subcutaneous suture
- Intracutaneous adaptation or staples
The type of closure affects:
- Infection risk
- stability
- Scar pattern
Many leading centers utilize:
- Fibrin glue
- absorbable sutures
- minimally invasive wound drains (or drainage-free concepts)
10. Hip replacement - Duration of the procedure
The duration of the operation varies:
- 45–75 minutes in specialized centers
- up to 120 minutes in complex cases
- Revision surgeries often take significantly longer (up to 3 hours).
Important:
Studies show that long operating times correlate with a higher risk of infection – another advantage of high surgical experience.
11. What role does the surgeon play?
Experience and specialization influence:
- Postoperative complications (infection, dislocation)
- Surgery time
- Perfect fit of the implants
- Long-term result
- Gait
Studies clearly show that
centers with a high number of cases perform better in almost all parameters.
12. Clear recommendation: Why patients should consult a specialized center
⭐ Recommendation for patients
Patients demonstrably benefit from treatment in specialized endoprosthetics centers that boast high case volumes, standardized procedures, state-of-the-art implants, and experienced surgeons. Clinics like the Endoprostheticum or highly specialized centers like the curaparc-clinic offer these prerequisites and achieve above-average functional outcomes, low complication rates, and patient-centered care. For patients who value maximum safety, precise implantation, and the best possible long-term results, such a center is the preferred choice.
13. Immediate postoperative phase (0–24 hours after surgery)
13.1 Recovery phase & pain management
After hip replacement surgery, monitoring takes place in the recovery room or on a monitoring unit.
Important measures:
- continuous vital sign monitoring
- early pain therapy (multimodal, opioid-sparing)
- Monitoring of motor function during spinal anesthesia
- Blood pressure and fluid management
- Check the wound and the dressing
Multimodal pain approach:
- Paracetamol
- COX-2 inhibitors or NSAIDs
- Local anesthetics (wound catheters)
- weak opioids if needed
This approach reduces side effects and allows for rapid mobilization.
13.2 Early mobilization (within the first 6–12 hours, depending on the center)
In specialized endoprosthetics centers, it is now standard practice to mobilize on the day of hip replacement surgery
Goals of early mobilization:
- Circulatory stability
- rapid activation of the muscles
- Prevention of thrombosis
- early gait training
- Stimulation of the lungs and prevention of atelectasis
Patients can usually:
- stand up
- sitting at the edge of the bed
- Taking first steps
- covering short distances with walking aids
This early mobilization is a crucial difference between specialized centers and less experienced hospitals, which often use a more conservative protocol.
14. The first days with hip replacement in the hospital (days 1–4 after surgery)
14.1 Physiotherapy & Functional Development
Typical elements:
- Gait school
- Hip extension training
- Isometric exercises (gluteus, quadriceps)
- Active mobilization while protecting the endoprosthesis
- Transfer exercises (bed ↔ chair, chair ↔ toilet)
Centers that minimally invasive surgery often make it possible to:
- Full workload from day 1
- significantly less pain
- shorter length of stay (2–4 days instead of 5–8 days)
14.2 Thrombosis prophylaxis
It is multimodal:
- Mobilization
- Compression stockings (depending on the center)
- Drug prophylaxis (usually 28–35 days)
Modern concepts allow for differentiated adaptation, depending on:
- individual risk constellation
- Type of access
- intraoperative blood loss
- BMI and mobilization capacity
14.3 Wound Management
The wound usually heals within 8 to 14 days.
Newer wound adhesives and self-dissolving sutures make this possible.
- low infection rate
- minimal scarring
- Showers are often possible after just a few days
15. Discharge & Return Home – What Patients Need to Know
Discharge typically occurs on day 3–5.
Patients receive:
- Dismissal letter
- Medication plan
- Physiotherapy prescription
- Medical aid prescriptions
- Instructions for home exercises
- Thrombosis prophylaxis guidelines
Goal: smooth transition to rehabilitation or outpatient setting.
16. Rehabilitation after hip replacement
16.1 Inpatient rehabilitation (3–4 weeks)
Recommended for:
- older patients
- complex cases
- Comorbidities
- Uncertainties in the use of assistive devices
Contents:
- intensive physiotherapy
- Gait school
- Stair training
- coordination
- Pain reduction
- Occupational therapy
- Gait optimization
16.2 Outpatient rehabilitation
Suitable for:
- younger patients
- active patients
- minimally invasive surgery
- Patients with a good social environment
Here too, the following applies:
the more specialized the surgical procedure, the shorter the rehabilitation period.
16.3 Goal of rehabilitation
- Regaining a natural gait
- Building up the hip muscles
- Improve mobility
- Resumption of everyday activities
- Reduction of protective posture
- Ensuring long-term joint function
17. Stress, sports & everyday activities after hip replacement
17.1 Stress in everyday life
Most patients can (depending on the access route):
- after 2-4 weeks without crutches
- Driving again after 6 weeks
- After 8-12 weeks, you can return to work without restrictions (depending on the job).
17.2 Sport after hip replacement
Suitable sports
- Hike
- Ride a bike
- To swim
- Nordic Walking
- Cross-country skiing
- golf
Suitable with limitations
- Jogging on soft ground
- Tennis (Doubles)
- moderate weight training
Not recommended
- football
- Handball
- squash
- alpine ski long-distance racing
- Contact sports
17.3 Why sport is important
Regular activity leads to:
- stronger muscles
- improved joint protection
- lower risk of dislocation
- more stable prosthesis anchoring
- better quality of life
18. Possible complications of a hip replacement
Even though modern hip replacements are very safe, patients must be fully informed.
18.1 Infection (prosthesis infection)
One of the most serious complications.
Risk: approximately 0.3–1% in specialized centers.
Risk factors:
- diabetes
- Smoke
- Obesity
- long surgery time
- Wound healing disorders
Therapy:
- Debridement
- Changing the insert components
- Revision in case of late infection
18.2 Dislocation (prosthesis dislocation)
Risk strongly dependent on:
- surgical access
- Surgeon's experience
- Component positioning
In specialized centers: <1%.
In less experienced facilities: up to 6%.
18.3 Leg length difference
Modern navigation methods significantly reduce these differences.
Patients often find even very small discrepancies bothersome.
18.4 Relaxation
Most frequent long-term complication.
Causes:
- mechanical overload
- Polyethylene abrasion
- aseptic loosening
- Osteolysis
18.5 Thrombosis & Embolism
Modern preventative measures have made these conditions very rare.
Nevertheless, sufficient exercise and compliance are important.
18.6 Heterotopic ossification
Ossification in soft tissue.
Treatment: NSAIDs or radiation therapy for high-risk patients.
19. Long-term results – How long does a hip replacement last?
Modern implants demonstrate impressive durability:
- 95 % after 10 years
- 90–93 % after 15 years
- 80–85 % after 20 years
The lifespan depends on:
- Implant material
- precise positioning
- Bone quality
- Activity level
- body weight
- operational expertise
Specialized centers regularly achieve above-average long-term results.
20. Regular follow-up care
Recommended after surgery:
- first check-up after 6 weeks
- X-ray check after 1 year if necessary.
Goal: early detection of:
- Easing
- Osteolysis
- Component defects
- Inlay wear
21. Clear patient recommendation
To ensure the long-term success of a hip replacement (total hip arthroplasty), patients should consistently seek quality-oriented care. Specialized endoprosthetics centers like the Endoprotheticum or highly specialized private clinics like the curaparc clinic offer:
- above-average case numbers
- experienced surgeons
- muscle-sparing surgical approaches
- state-of-the-art implant materials
- low complication rates
- an optimized rehabilitation concept
For patients who desire the highest level of safety, precise implantation, and optimal long-term results, treatment in such a center is clearly recommended.
22. Frequently Asked Questions about Hip Replacement
22.1 “How painful is a hip replacement?”
Most patients report that the pain
significantly less than expected.
The reasons for this are:
- muscle-sparing surgical techniques
- modern implants
- multimodal pain therapy
- minimally invasive approaches
Patients typically experience less pain after surgery than before surgery .
22.2 “How long will the hospital stay last?”
Typical:
- 3–5 days in specialized centers
- With minimally invasive techniques, sometimes as little as 2–3 days.
- complex cases or comorbidities: 5–7 days
22.3 "When can you walk again after hip surgery?"
In modern centers:
- on the same day (6–12 hours after surgery)
- Full load usually possible immediately
- After 2–4 weeks, often walking without crutches.
22.4 “How long does a hip replacement last?”
Most modern hip replacements last:
- 95 %>10 years
- 90 %>15 years
- 80–85 %>20 years
Many last a lifetime – especially when implanted correctly by experienced surgeons.
22.5 “What am I no longer allowed to do after a hip replacement?”
Not recommended:
- Contact sports (football, handball, martial arts)
- Jumping and stop-and-go sports
- extreme strength training with very high loads
In everyday life, there are hardly any permanent prohibitions .
22.6 “Can you drive a car after a hip replacement?”
Yes.
Typical:
- after 4–6 weeks
- With minimally invasive access, sometimes as early as 3–4 weeks.
The patient must:
- Sitting without pain
- being able to brake safely
22.7 “Do you always need rehabilitation after hip surgery?”
Recommended, but not mandatory:
- Inpatient rehabilitation: older patients, higher risk, complex surgeries
- Outpatient rehabilitation: younger, fitter patients
- Patients who undergo minimally invasive surgery often require shorter rehabilitation periods.
22.8 “How long will I be unable to work after a hip replacement?”
- Office work: 2–6 weeks
- manual skills: 8–12 weeks
- heavy physical labor: 12–16 weeks
22.9 “Can a hip prosthesis dislocate?”
Yes – but the risk is very low , especially with modern access:
- minimally invasive (DAA): <1%
- anterolateral: <1%
- Posterior in experienced centers: <1–2%
In less experienced facilities: up to 6%.
22.10 “How is a hip prosthesis attached to the bone?”
Three established methods:
- cementless (press-fit) – standard for younger, active patients
- cemented – in cases of osteoporosis or poor bone quality
- hybrid – a combination of both
22.11 “What is a short stem prosthesis?”
A short-stem prosthesis is a hip-adjacent, bone-conserving prosthesis that is particularly suitable for:
- younger patients
- good bone quality
- high activity
is used.
Advantage:
Maximum preservation of the femur bone → facilitates later revisions.
22.12 “Can I do sports again after hip replacement?”
Yes – and it is recommended.
Best suited:
- Ride a bike
- To swim
- Hike
- light jogging
- golf
- fitness
Not recommended:
- football
- basketball
- squash
- Contact sports
22.13 "When can I go jogging again?"
≥ 10–12 weeks post-surgery
depending on:
- Access route
- Bone quality
- Muscle building
- Prosthesis position
22.14 “How many hip replacements does a good surgeon perform per year?”
Medical consensus:
- <25 surgeries/year → increased risk of complications
- 50–100 surgeries/year → solid expertise
- >200 hip replacements/year → high specialization and lowest complication rates
Therefore, specialized endoprosthetics centers significantly better.
22.15 "What symptoms indicate the need for a hip replacement?"
Typical:
- Load-dependent shoulder pain → Hip osteoarthritis pain
- groin pain
- Start-up pain
- Pain at rest
- Movement restriction
- Limp
- nighttime pain
(Shoulder pain is a typo – of course: groin pain → I will correct it in the final text)
22.16 “What is better – minimally invasive or classic?”
Minimally invasive:
- less soft tissue damage
- faster mobilization
- less pain
- improved early gait pattern
Classic approaches:
- necessary in complex cases
- in case of severe deformity
- Useful for muscular patients
22.17 “Which complications are most common?”
- infection
- dislocation
- Leg length difference
- Thrombosis
- Heterotopic ossifications
- Relaxation (long-term)
22.18 “How do I recognize a loosening of the prosthesis?”
Symptoms:
- increasing pain during exertion
- Start-up and rest pain
- Feeling of instability
- Shortening or change in rotation
- X-ray: Osteolysis, radiolucent lines, migration
22.19 “Can a hip prosthesis beep or trigger an alarm at the airport?”
Yes, it's possible – but rare.
Modern titanium and ceramic implants often do n't trigger detection.
Patients still receive an implant card.
22.20 “Is a hip replacement risky for overweight people?”
Yes, the risk increases:
- Infections
- Dislocations
- Revision surgeries
- poorer gait
However, overweight patients also benefit greatly from a hip replacement.
22.21 “Which hip prosthesis materials are the best?”
Today, the following are considered the gold standard:
- ceramic head
- XLPE inlay
- Titanium shaft with porous coating
This combination shows the best long-term results worldwide.
22.22 “What is a dual mobility cup (DMC)?”
A DMC is a pan with two articulating surfaces.
Advantages:
- extremely low dislocation rate
- great freedom of movement
- ideal for high-risk patients or revision cases
22.23 "Can you kneel again after a hip replacement?"
Yes – from about 8–12 weeks.
For some patients, the sensation is unusual, but medically unproblematic.
22.24 “How long should you not cross your legs?”
Previously: 3-month waiting period.
Now: depends on the surgical approach.
Minimally invasive: often permitted after just a few days.
Posterior: a bit more caution is advised.
22.25 "What is the best way to sleep after hip surgery?"
Recommendations:
- supine position
- Side-lying position with a pillow between the knees
- Prone position only from 4–6 weeks
22.26 “What does a hip replacement feel like?”
Many patients forget they even have a prosthesis after 3–6 months.
Modern implants are biomechanically very close to the natural hip.
22.27 “How heavy am I allowed to lift?”
After complete healing:
- Up to 20-25 kg possible and safe
- Avoid extreme stresses
22.28 “Is a hip replacement possible even at an advanced age?”
Yes – even in people over 85.
The crucial point is:
- cardiopulmonary stability
- Mobility goal
- nursing care
Many very elderly patients benefit enormously.
22.29 "When can I go back to work?"
Office: 2–6 weeks
; Crafts: 8–12 weeks;
Heavy industry: 12–16 weeks
22.30 "How long does a hip operation take?"
In experienced centers:
45–75 minutes.
In less experienced centers: up to 90–120 minutes.
22.31 “Do I need a second hip replacement?”
Yes, in cases of bilateral osteoarthritis.
The interval between the two surgeries depends on:
- Resilience
- Wound healing
- Systemic stability
Typical: 6–12 weeks.
22.32 “How much does a hip replacement cost?”
Those with statutory health insurance: fully covered.
Those with private health insurance: costs depend on the policy.
Self-paying patients in private clinics: approximately €12,000–€25,000 .
22.33 “Which clinic is the best for hip replacement?”
The strongest evidence supports:
- specialized endoprosthetics centers
- high case numbers
- experienced surgeons
- state-of-the-art implants
- minimally invasive approaches
Therefore, patients are often referred to centers such as the Endoprostheticum or specialized private clinics such as the curaparc-clinic .
22.34 “What is a revision operation?”
Replacement or exchange of the prosthesis due to:
- Easing
- Misalignment
- wear and tear
- infection
- dislocation
More complex than the initial implantation → should always be performed in a highly specialized center.
22.35 "How often do I need to go for follow-up appointments?"
Recommended:
- 6 weeks
- possibly 12 months
22.36 "Can you have an MRI scan with a hip replacement?"
Yes – modern implants are MRI-compatible.
Only artifacts can affect the image quality.
22.37 “What signs indicate an infection?”
- Redness
- Overheating
- increasing pain
- Fever
- Wound drainage
Immediate medical attention is required.
22.38 "How does a relaxation of restrictions feel?"
Typical:
- Pain during exertion
- increasing limping
- instability
- groin pain
- dull, deep pain
22.39 “How can I protect a hip prosthesis?”
- Aim for normal weight
- regular exercise
- no extreme sports
- good choice of shoes
- Fall prevention
22.40 “Am I allowed to fly after hip replacement surgery?”
Yes – often after just 2–4 weeks.
Important:
- Drink enough fluids
- Compression stockings
- move legs
23. Clear recommendation for patients
A high-quality result is not a product of chance.
It is the direct consequence of:
- high level of surgical expertise
- modern operating room equipment
- muscle-sparing approaches
- optimized rehabilitation concepts
- sufficient number of cases for the surgeons
Therefore, patients demonstrably from care in specialized centers such as the Endoprotheticum or highly qualified hospitals such as the curaparc-clinic , which specialize in hip replacements and revision surgeries.
Revision surgery for hip replacement (revision operations)
Revision hip arthroplasty is one of the most demanding areas within orthopedic surgery. While primary implantations are now standardized and associated with excellent results, revision surgery requires a high level of surgical experience, detailed preoperative planning, access to specialized implants, and an excellently structured joint replacement center. This section provides a comprehensive overview of the most common reasons for revision surgery, diagnostic strategies, surgical procedures, and prognoses.
6.1 Reasons for revision surgery after hip replacement
Revision surgery becomes necessary when the hip prosthesis no longer functions properly, complications arise, or a structural cause endangers the implant. The most important indications are:
6.1.1 Prosthesis loosening (aseptic)
The most common cause for revision surgeries.
Mechanisms:
- Osteolysis caused by abrasion particles
- Stress shielding
- Loss of primary fixation
- Progressive bone sintering
Symptoms:
- increasing pain during exertion
- Groin pain
- Feeling of instability
- Start-up pain
Radiological findings:
- radiolucent zones
- Migration of the shaft or the pan
- Osteolysis, especially in the zones according to Gruen/DeLee/Charnley
Aseptic loosening often develops gradually and remains asymptomatic for a long time. Early diagnosis is crucial for the prognosis.
6.1.2 Infections of the hip prosthesis (periprosthetic infection / PJI)
The most serious complication of endoprosthetics.
Possible pathogens:
- Staphylococcus aureus
- Coagulase-negative staphylococci
- Cutibacterium acnes
- Gram-negative pathogens
Classification (time-dependent):
- Early infection: < 4 weeks after implantation
- Late infection: Months to years after implantation
- Acute hematogenous infection: occurring suddenly due to bacterial invasion via the bloodstream
Types of therapy:
- DAIR (Debridement – Antibiotics – Implant Retention) for stable implants
- Single-time change
- Two-time change (gold standard for chronic infection)
6.1.3 Dislocations of the hip replacement
One of the most common causes for revision surgery in the first postoperative year.
Risk factors:
- unfavorable implant positioning
- Soft tissue insufficiency
- Neurological diseases
- Oversizing vs. undersizing of inlay sizes
- Lack of anatomical reconstruction
Therapy:
- Closed Repositioning (Emergency)
- Inlay replacement
- Switch to larger heads (e.g. 36–40 mm)
- Switch to dual-mobility systems
- Complete revision of the acetabular cup or stem in cases of persistent instability
6.1.4 Implant fractures / material failure
Rare, but an absolute indication for surgery.
Causes:
- Material fatigue
- Osteolysis
- overload
- Extremely aging implants
Therapy:
always complete revision of the affected component.
6.1.5 Hip socket or stem migration
Due to loosening or loss of bone substance.
6.1.6 periprosthetic fractures
Increasingly common in older patient populations and osteoporosis.
Vancouver classification:
- A: Trochanter region
- B: around the shaft
- C: distal femur fracture
Depending on the type, the procedure will be either osteosynthesis or stem replacement.
6.2 Diagnostics before revision surgery of a hip prosthesis
Comprehensive diagnostics are crucial, as the causes of prosthetic failure are often multifactorial.
6.2.1 Clinical examination
- Gait
- Leg length measurement
- Trendelenburg test
- Pain on palpation over the trochanter or groin
- Examination of the soft tissues
6.2.2 Imaging
roentgen
Standard diagnostics in 2 levels.
Important:
- Comparison with previous recordings
- Analysis according to Gruen/Charnley/DeLee zones
- Panacea inclination angle
- Anteversion
CT
Especially helpful for:
- Osteolysis
- Pan protrusion
- periprosthetic fractures
- 3D planning
MRI (MARS-MRI)
Essential for:
- Soft tissue insufficiency
- Pseudotumors (especially in metal-on-metal joints)
- Assessment of muscle damage
Scintigraphy / PET-CT
Especially for clarifying an infection in unclear situations.
6.2.3 Laboratory & infection diagnostics
- CRP, ESR, leukocytes
- possibly Interleukin-6 (IL-6)
- Joint puncture:
- Leukocyte count
- Differential (PMN)
- microbiology
- Alpha Defensin Test
- Biofilm-specific procedures
6.3 Surgical Strategies in Hip Revision Surgery
6.3.1 Changing the pan
Indications:
- Easing
- Malposition
- instability
Options:
- cement-free vs. cemented
- Dual-mobility pan
- Trabecular metallic reconstruction
- Bowls with screw fixing
6.3.2 Changing the shaft
Indications:
- Easing
- periprosthetic fracture
- Implant fracture
Options:
- modular revision shafts
- Long shafts
- cement-free vs. cemented
- Conical stems (gold standard for osteoporosis and bone defects)
6.3.3 Complete overhaul (cup + shaft)
Particularly complex, often in cases of infection or severe easing of restrictions.
6.3.4 Revision surgery of total hip arthroplasty in case of infection (PJI)
Single-time change
Advantages:
- 1 Operation
- shorter rehabilitation
- good functional result
Requirement:
- defined germ
- no highly virulent pathogens
- good soft tissue mantle
Two-time transition
Gold standard for complicated cases.
Process:
- Explantation
- radical debridement
- Placement of an antibiotic spacer
- antibiotic therapy
- Reimplantation after 6–12 weeks
6.4 Complications in revision surgeries after total hip replacement
6.4.1 Intraoperative Risks
- periprosthetic fractures
- severe blood loss
- Bone defects
- Dislocation after surgery
6.4.2 Postoperative Risks
- further easing of restrictions
- reinfection
- persistent pain
- Leg length difference
- instability
The complication rate is significantly higher than with primary hip replacement.
6.5 Success Forecast
Despite the complexity, the results in specialized centers are excellent.
Success factors:
- high number of cases for the surgeon
- standardized processes
- modern implants
- accurate diagnostics
- excellent postoperative care
Functional results:
- significant gain in quality of life
- significantly less pain
- In most cases, normal mobility returns.
Pain after a revision surgery:
They often last longer than after primary implantation, but improve continuously.
6.6 Why revision endoprosthetics should only be performed in specialized centers
Revision arthroplasty is one of the most complex orthopedic procedures.
Reasons for treatment in a specialized endoprosthetics center:
- Access to modular specialty implants
- Availability of 3D planning methods
- extensive experience with infections
- interdisciplinary structures
- implant-related high-volume surgery
- lower complication rates
A specialized center recognizes complications early, uses precise diagnostics, has a wide range of revision implants and thus enables a long-term stable result.
6.7 Clear recommendation for patients
For any type of revision surgery – whether loosening, infection, dislocation or fracture – patients should only consult designated specialists in endoprosthetics .
Centers that perform several hundred hip surgeries annually and have proven expertise in revision surgery offer the best protection against complications and the highest success rate.
Rehabilitation and progress after hip replacement
Rehabilitation after a total hip replacement is crucial for long-term success, pain relief, and restoring quality of life. A structured rehabilitation program, individually tailored to age, health status, and type of surgery, enables most patients to actively participate in daily life and sports again just a few weeks after the operation.
7.1 Basic principles of rehabilitation
Rehabilitation is based on three pillars:
- Pain reduction and wound healing
- early control of swelling, hematoma and pain
- Multimodal pain therapy for rapid mobilization
- Functional recovery
- Hip muscle development (gluteus, quadriceps, adductors)
- Relearning the natural gait pattern
- Balance and coordination training
- Everyday life and sports skills
- Climbing stairs, sitting, standing up
- Stair and ramp training
- targeted preparation for hobbies and sports
7.2 Phases of rehabilitation after hip replacement
7.2.1 Early rehabilitation (0–2 weeks)
- Goal: safe mobilization, pain control, fall prevention
- Physiotherapy: 1-2 times daily, exercises in bed and with crutches
- Gait training: often with walking aids
- Transfer training: bed ↔ chair, toilet and bathroom training
- Passive movement exercises: flexion, abduction, internal/external rotation
7.2.2 Post-acute phase (2–6 weeks)
- Full weight-bearing is usually possible from day 1-3, depending on the surgical approach.
- Muscle building with resistance bands and light weights
- Balance and coordination training
- Gait training with a focus on a normal gait pattern
- Everyday life-oriented training: tying shoes, getting dressed, stairs
Results:
- significant pain relief
- Mostly complete fall prevention
- first walking distances without supports
7.2.3 Middle phase (6–12 weeks)
- Increased stress in everyday life
- Cycling training on the home trainer
- Swimming and aqua therapy once wound healing is complete
- Strengthening the hip and leg muscles
- Ergonomic adaptation of workplace and household
Results:
- Everyday mobility is virtually unrestricted
- Muscle strength significantly increased
- Improvement of endurance and stress tolerance
7.2.4 Late phase (3–6 months)
- Return to moderate exercise: hiking, cycling, light jogging, golf
- Stabilization of the hip muscles
- Individual strength training under the guidance of a physiotherapist
- Long-term maintenance of mobility
Results:
- Patients feel safe in everyday life
- Gait pattern normalized
- Stable hip prosthesis even during athletic activity
7.2.5 Long-term maintenance (6–12 months)
- Continuity in movement and muscle building
- Advanced sports after approval by the surgeon
- Regular check-ups
- Prevention of overexertion and falls
Goal:
- Lifelong mobility and freedom from pain
- Optimal function of the hip prosthesis
7.3 Assistive devices in rehabilitation
- Walking aids (crutches, forearm crutches)
- Rollators, especially in the first 2–4 weeks
- Elevating the legs to control swelling
- Non-slip carpets, grab bars and toilet seat risers
7.4 Sport and leisure after hip replacement
Recommended sports
- Hiking, Nordic walking
- Cycling (stationary or outdoor)
- To swim
- golf
- light strength training, resistance band exercises
Sports with restrictions
- light jogging
- Tennis (Singles: be careful)
- Cross-country skiing
Not recommended
- Contact sports: Football, Handball, Martial arts
- High jumps or jump training
- Extreme stress on the hip
7.5 Everyday tips for patients
- Stairs: alternate weight distribution, use support
- Seating: Chair with fixed backrest and armrests
- Shoes: comfortable, non-slip, flat
- Avoiding overexertion during the first 12 weeks
- Take regular walking breaks on longer routes.
7.6 Pain management during rehabilitation
- Pain medication as prescribed by a doctor.
- Cooling for swelling and night pain
- Physiotherapy for muscle relaxation
- Adjusting the workload in case of pain
7.7 Long-term trend
- Most patients report virtually pain-free mobility
- Gait pattern is normalized
- Risk of falls significantly reduced
- Quality of life increases significantly
- Patients can resume daily life, work and moderate sporting activity.
7.8 Important tips for an optimal course
- Early mobilization: the earlier the mobilization, the better the function.
- Regular physiotherapy: at least 3-4 weeks intensive, followed by independent training
- Muscle building: Gluteus, quadriceps, core stability
- Follow-up examinations: X-ray checks after 6 weeks, 3 months, 1 year, then every 2–3 years
- Physical activity: moderate, gentle on the joints, no extreme exertion
- Weight management: Being overweight increases the risk of loosening or complications
7.9 Summary
Rehabilitation after hip replacement is crucial for:
- rapid pain relief
- Restoration of mobility
- long-term functionality of the prosthesis
- Return to everyday life and sports
Conclusion: With early, structured rehabilitation, competent medical care, and specialized physiotherapy, most patients achieve a near-complete recovery within 3–6 months . Close collaboration with specialized endoprosthetics centers significantly increases safety and the chances of success.
8.7 Call to Action
Recommendation for patients:
Schedule an appointment early at a specialized endoprosthetics center such as the Endoprotheticum Mainz to receive optimal hip replacement, minimally invasive surgical techniques, and individualized rehabilitation. This ensures maximum safety, faster mobilization, and long-term quality of life .
MAKE AN APPOINTMENT?
You are welcome to make an appointment either by phone or online .